Slug
syncope
Video
Category
General Neurology
Excerpt
Syncope is another word for fainting. It is a clinical syndrome in which transient loss of consciousness (TLOC) is caused by inadequate blood flow to the brain, most often the result of an abrupt drop of systemic blood pressure. A person with syncope typically recovers quickly without treatment. Typically, syncope is not a sign of a life-threatening problem, although some people with syncope do have a serious underlying medical condition.
Authors
Tags
Featured
Featured
Ready to Publish
Ready to Publish
Publish Date
Nov 16, 2022
Introduction
Syncope is another word for fainting. It is a clinical syndrome in which transient loss of consciousness (TLOC) is caused by inadequate blood flow to the brain, most often the result of an abrupt drop of systemic blood pressure. A person with syncope typically recovers quickly without treatment. Typically, syncope is not a sign of a life-threatening problem, although some people with syncope do have a serious underlying medical condition.
.png)
Pre-syncope or prodome is the feeling of passing out. Pre-syncope symptoms include lightheadedness (dizziness), nausea, feeling unsteady in upright position, visual "graying out," trouble in hearing or occurrence of unusual sounds, palpitations, weakness, or a sudden sweating, and pallor. Loss of consciousness does not happen during pre-syncope. Pre-syncopal episodes should also be mentioned when talking to your doctor about syncope. Younger people with the vasovagal form of reflex syncope experience this more frequently than elderly patients or those with syncope from other causes.
Causes of syncope
Some of the most common medical conditions that cause syncope are the following:
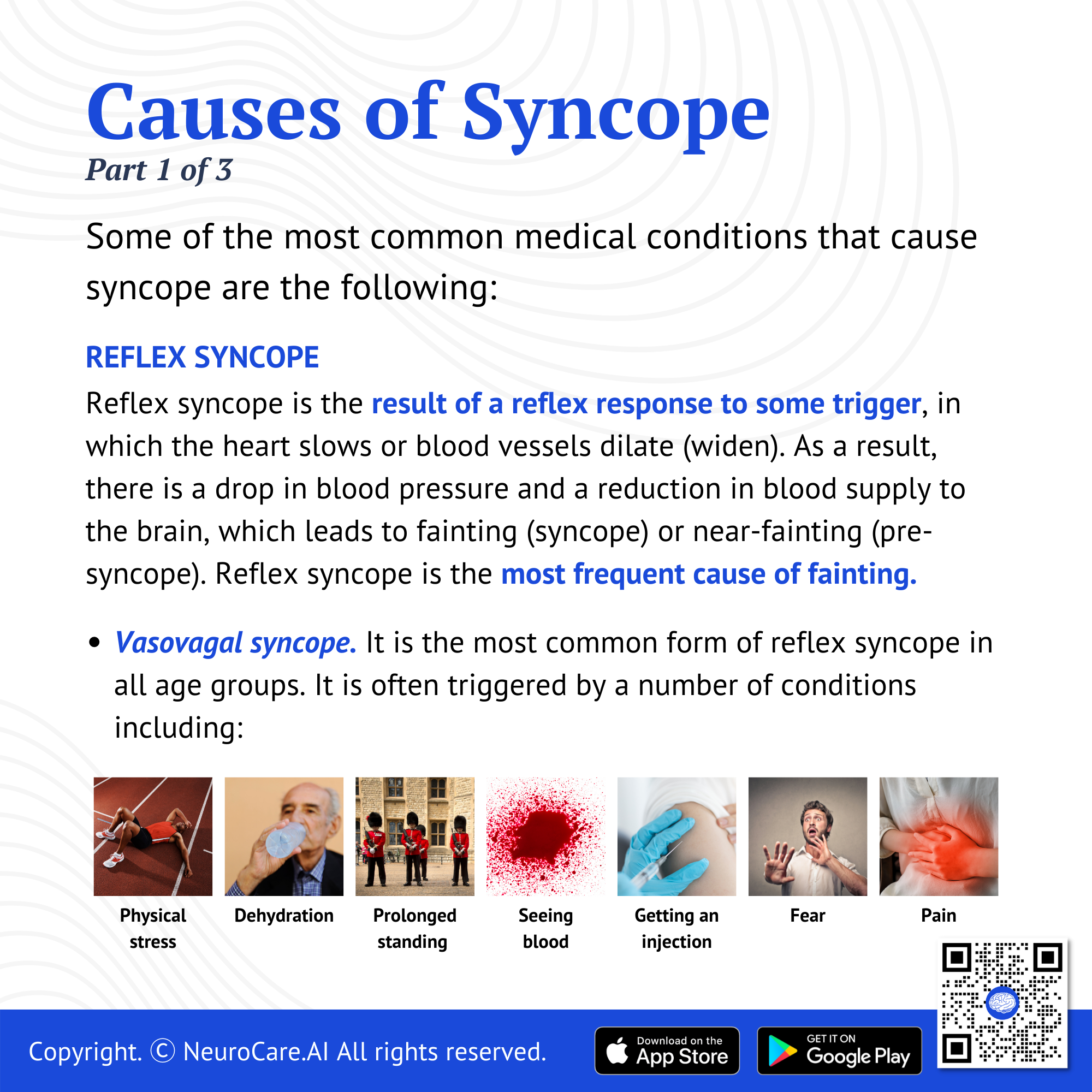
Reflex syncope
Reflex syncope is the result of a reflex response to some trigger, in which the heart slows or blood vessels dilate (widen). As a result, there is a drop in blood pressure and a reduction in blood supply to the brain, which leads to fainting (syncope) or near-fainting (pre-syncope). Reflex syncope is the most frequent cause of fainting.
- Vasovagal syncope
It is the most common form of reflex syncope in all age groups, but especially in younger people. Vasovagal syncope is often triggered by a number of conditions including physical stress, dehydration, bleeding, standing up quickly, standing upright for a long time, and emotions in response to stimulus like seeing blood, getting an injection or having blood drawn, fear, and pain.
During a vasovagal syncope, the blood pools in the lower extremities and the bowels, which reduces the amount of blood returning to the heart and lowers blood pressure (hypotension). This results in decrease in blood flow to the brain which causes near or complete loss of consciousness. Blood flow is restored when the person falls down or is placed in a horizontal position.
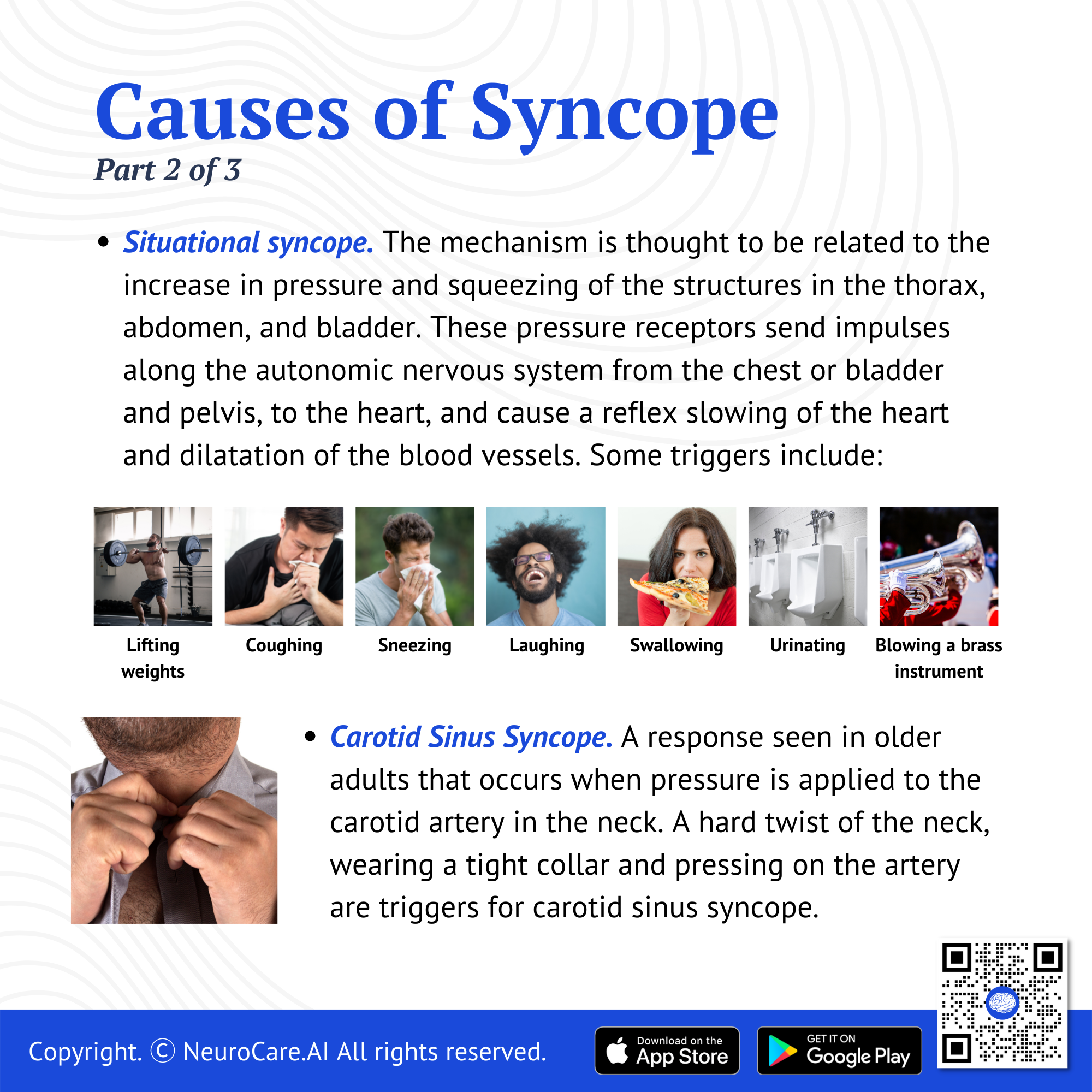
- Situational syncope
There are several unusual situations that may provoke a syncope. The mechanism is thought to be related to the increase in pressure and squeezing of the structures in the thorax, abdomen, and bladder. These pressure receptors send impulses along the autonomic nervous system from the chest or bladder and pelvis, to the heart, and cause a reflex slowing of the heart and dilatation of the blood vessels. Some triggers include coughing, sneezing, laughing, swallowing, pressure on the chest after exertion or exercise, defecating, urinating, eating a meal, sudden abdominal pain, blowing a brass instrument, and lifting weights.
- Carotid Sinus Syncope
A response seen in older adults that occurs when pressure is applied to the carotid artery in the neck. A hard twist of the neck, wearing a tight collar and pressing on the artery are triggers for carotid sinus syncope.
.png)
Orthostatic Hypotension
Orthostatic hypotension refers to low blood pressure that occurs when a person is in upright position such as standing or siting up. Fainting results from inadequate blood flow to the brain due to more blood circulating to the lower part of the body because of the effects of gravity. Orthostatic hypotension is common in elderly and is frequently made worse by dehydration or medications that lower blood pressure, such as diuretics.
Heart rhythm problems
Syncope can result from a variety of heart rhythm and/or rate problems. These disturbances are called arrhythmias. Cardiac syncope often occurs suddenly, without dizziness or other pre-syncope symptoms.
There are other reasons that a person may pass out. Examples of non-syncopal causes of TLOC or apparent TLOC include seizure, cardiac arrest, sleep disturbances, incidents resulting in traumatic brain injury, intoxications and metabolic disturbances like low blood sugar level, and some psychiatric conditions. These are not syncope but are important to assess and prevent.
.png)
Diagnosing syncope
It’s important to determine the source of syncope to rule out potentially dangerous heart problem, if possible. The following tests may be used to determine the cause, depending on your symptoms and circumstances:
- Comprehensive history. It is essential to obtain information about the syncope episode(s) and past medical history to determine whether apparent transient loss of consciousness (TLOC) episodes are true syncope or the result of some other cause of the collapse.
- Physical examination. Physical examination findings such as abnormalities in vital signs, cardiovascular disturbances, and neurologic symptoms might help identify some of the major causes of syncope.
- Electrocardiogram (ECG). An ECG should be obtained in all patients with suspected syncope. Though 12-lead ECG rarely pinpoints an exact arrhythmic cause of syncope, some results can be very helpful.
- Transthoracic echocardiogram. Echocardiographic results can be utilized to determine whether structural heart disease is present in syncope patients, but rarely offer a precise causative diagnosis, as another potential diagnosis may be contributing.
- Exercise stress test. This is done with ECG recording while the patient is having strenuous exercise.
- Tilt table test. This test simulates the sudden changes in posture in a controlled situation, then the patient’s heart rate and blood pressure are measured in response to an upright tilt.
Treatment of syncope
The treatment for syncope will depend upon the underlying condition. The treatment goal is to prevent recurrences or more serious problems.
Vasovagal syncope treatment. Vasovagal syncope may typically be managed by taking precautions to avoid potential triggers and reduce the chance of injury. Lying down and elevating the legs when you feel that you will pass out will prevent syncope to happen.
Counter-pressure maneuvers. A vasovagal syncopal episode may be stopped by counter-pressure techniques, or at least delay it long enough for you to lie down with your feet elevated. Examples of these maneuvers are:
- Leg crossing while tensing the leg, abdominal, and buttock muscles.
- Hand gripping, which involves gripping a rubber ball or similar object as hard as possible.
- Arm tensing, which involves gripping one hand with the other while simultaneously moving both arms away from the body.
Orthostatic training. Also called standing training. Orthostatic training may help persons with orthostatic hypotension and vasovagal syncope have fewer chances of syncope. Methods to reduce blood pooling in the extremities, which prevent your blood pressure to fall when you stand, are applied such as the following:
- Wearing elastic compression stockings on the feet and lower legs
- Contraction of the leg muscles before and while standing
- Rising to stand slowly and in stages
Cardiac syncope management. If a cardiovascular cause is identified, medications may be prescribed and surgical procedures may be done to control heart rhythm.
Syncope and safety
Syncope is generally associated with physical collapse which may result in injury due to a fall or other type of accident. Passing out while driving or other activities can potentially harm both the person and those around them. Driving limitations are sometimes advised for specific syncope patients and other people who have a history of syncope that happens suddenly or for no apparent cause.
Visit your doctor
Consult your doctor if syncope happened to you suddenly, if it became more frequent, or an episode lasted longer before full recovery.
Take note of the number, frequency, and duration of the syncopal episodes. A patient who experienced multiple episodes occurring over a short period of time is more likely to be suffering from a serious underlying disorder. Longer periods of apparent or actual loss of consciousness, especially if they last longer than five minutes, may indicate that the occurrence is not syncope or is not syncope alone.
DISCLAIMER:
The information in this document is for general educational purposes only. It is not intended to substitute for personalized medical professional advice. NeuroCare.AI makes every effort to provide accurate and timely information, but makes no guarantee in this regard and disclaims responsibility for adverse consequences resulting from its use. For further information, consult a physician and the organization referred to herein.
AizaMD™: Revolutionizing Clinical Documentation
Discover the power of our ambient clinical documentation system, designed to transform clinical encounters into structured SOAP notes with unmatched ease. Experience exceptional value for less than $3 per day—cheaper than your daily coffee!
- Save Time: Free up over 90 minutes daily for each provider.
- Boost Revenue: Increase daily revenue by at least $1,000 per provider.
- Enhance Coding Quality: Our detailed documentation supports superior coding accuracy, ensuring optimal reimbursement.
- Maximize Engagement and Interaction: Dedicate more time to patient care and less to typing, fostering richer and more effective conversations between clinicians and patients
AizaMD™: Automated Radiology Report Generation!
Discover our breakthrough Radiology AI reporting platform built on Ambient AI. It enhances productivity and minimizes fatigue. Benefit from best-in-class accuracy with our automated radiology report generation, all at market-leading pricing.
📈 Efficiency: Cut dictation times by up to 50% (Less words, More report!
🎯 Focus: Keep your eyes on the images, not the keyboard!
💸 Revenue: Boost revenue by at least 20%
📑 Clarity: Patient summary in plain English