Slug
migraine-headache
Video
Category
Headache
Excerpt
Migraines are also used to describe headaches, however, they are much more chronic and have a localised effect. It is also a condition that occurs only in a specific area of the head. Globally, it is one of the leading causes of disability and it is the second leading cause of death. There is a genetic link between migraine and migraine sufferers. Let us take a close look at the causes and symptoms of migraine headache and other factors that contribute to the disorder.
Authors
Tags
Featured
Featured
Ready to Publish
Ready to Publish
Publish Date
Sep 19, 2022
Introduction
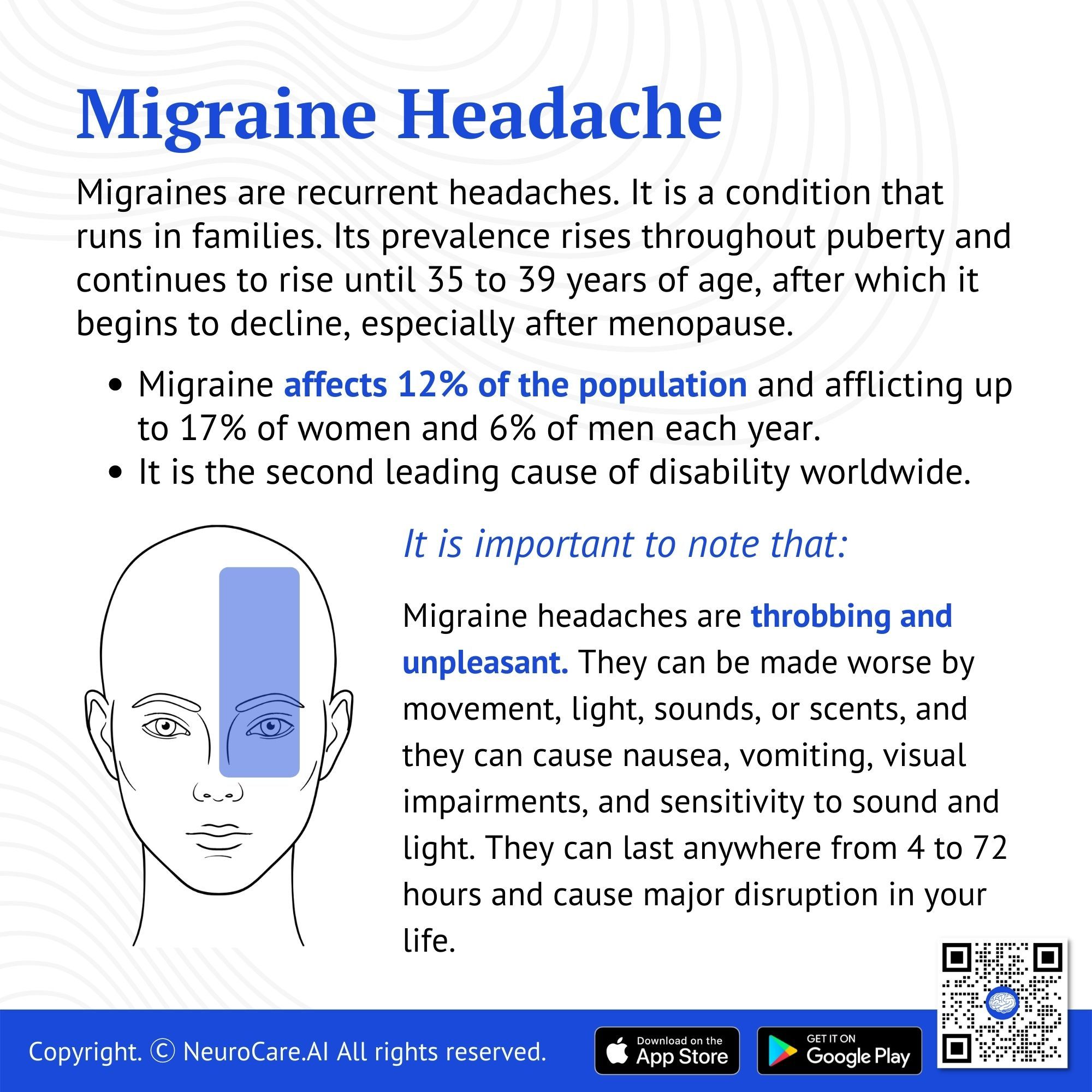
Migraine is quite common, affecting 12% of the population and afflicting up to 17% of women and 6% of men each year. It is the second leading cause of disability around the globe. Migraine is a condition that runs in families. Its prevalence rises throughout puberty and continues to rise until 35 to 39 years of age, after which it begins to decline, especially after menopause. It is more common than diabetes, epilepsy, and asthma combined. Moderate, consistent exercise can help to lessen the frequency of episodes.
Migraines are recurrent headaches caused by changes in the brain and surrounding vascular system. In most cases, it is accompanied by an aura (changes in vision and sense of smell). The severity of migraine headaches can range from mild to severe, with throbbing and unpleasant symptoms. Symptoms include nausea, vomiting, visual impairments, and sensitivity to light and sound. Movement, light, sounds, or scents can aggravate them. There is a great deal of pain and acuteness associated with migraines, compared to regular tension headaches. It can last between four and 72 hours and cause major disruptions in your life.
🧠 Key Insights:
- There is about three times as many women suffering from migraines as men.
- About 10% of school-age children suffer from migraines.
- There is a 50% increased risk of getting migraines as a child when one or both of your parents have a history of migraines.
- If a person suffers from at least 15 migraines a month, they are deemed to be chronic sufferers of migraines.
- It is estimated that there are 39 million Americans with migraines.
What are the Symptoms of a Migraine?
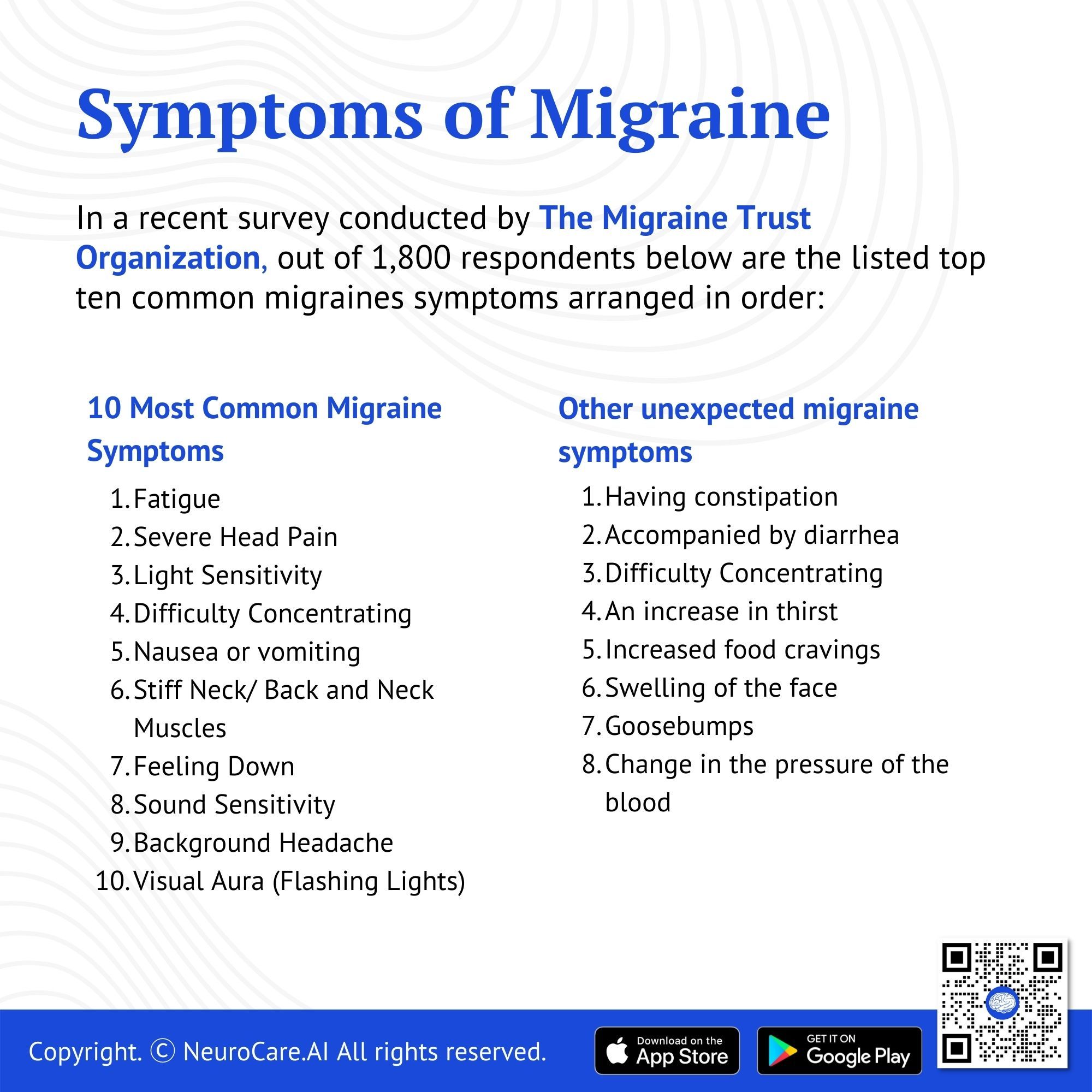
In a recent survey conducted by The Migraine Trust Organization, out of 1,800 respondents below are the listed top ten common migraines symptoms arranged in order:
10 Most Common Migraine Symptoms
- Fatigue
- Severe Head Pain
- Light Sensitivity
- Difficulty Concentrating
- Nausea or vomiting
- Stiff Neck/ Back and Neck Muscles
- Feeling Down
- Sound Sensitivity
- Background Headache
- Visual Aura (Flashing Lights)
Other unexpected migraine symptoms
Some other unexpected migraine symptoms include:
- Having constipation
- Accompanied by diarrhea
- Difficulty Concentrating
- An increase in thirst
- Increased food cravings
- Swelling of the face
- Goosebumps
- Change in the pressure of the blood
What Causes Migraines?
The blood arteries in your head tighten and enlarge during a migraine, causing pain. A migraine can be triggered by physical or mental stress, as well as particular meals. Migraines can be brought on by a number of things. Food and drink triggers, sleep habits, hormones, and tightness, particularly in the neck, are all examples of stress (and how stress is handled). However, the specific cause is unknown.
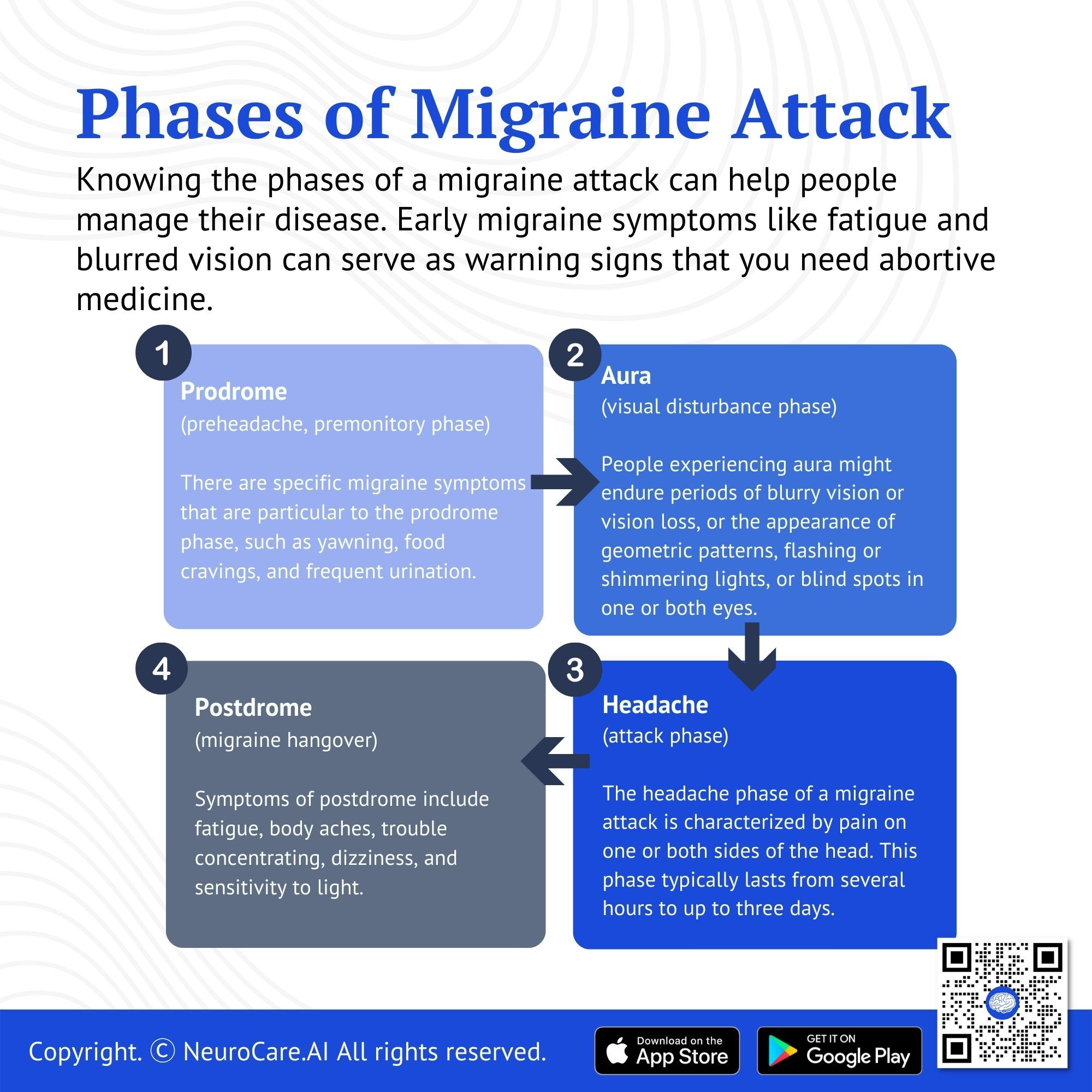
Phases of a Migraine Attack
Knowing the phases of a migraine attack can help people manage their disease. Early migraine symptoms like fatigue and blurred vision can serve as warning signs that you need abortive medicine. Some people can even avoid migraines by identifying and treating them early. In addition, identifying risk factors that can cause postdrome "hangovers" may help people anticipate how long it is going to last.
- Prodrome
Prodrome, also known as "pre-headache" or the premonitory phase, is the first phase of a migraine attack. This phase may last several hours or even several days.
A prodrome usually precedes migraine attacks, though not necessarily every migraine attack. In order to lessen the severity of the coming headache, an individual experiencing prodrome may be evaluated by his or her care team to guide a treatment plan. Mood changes, irritability, or depression may be symptoms of the prodrome, which can vary from person to person. There may also be fatigue, sensitivity to light and sound, insomnia, nausea, constipation, diarrhea, and muscle stiffness, especially in the neck and shoulders. Certain migraine symptoms are specific to the prodrome phase, such as yawning, food cravings, and frequent urination. It has been shown that taking medication, minimizing/avoiding other trigger factors (e.g. foods, alcohol), and engaging in mindfulness meditation, relaxation therapy, or other biobehavioral techniques during this phase can even prevent headaches in some cases.
- Aura
Up to one-third of people with migraine experience aura as a distinct phase in the progression of their migraine attack. Like other phases, the aura doesn’t necessarily occur during every migraine attack in those who experience them. People experiencing aura might endure periods of blurry vision or vision loss, or the appearance of geometric patterns, flashing or shimmering lights, or blind spots in one or both eyes. These symptoms usually gradually evolve over at least 5 minutes and can last for up to 60 minutes. Not all auras are followed by headaches, but since they typically precede the headache phase, they can serve as another warning of a potential headache. In about 20% of individuals, the aura may last longer than 60 minutes and in some, the aura may not precede the headache phase but occur after the headache has already started.
3. Headache
The headache phase of a migraine attack is characterized by pain on one or both sides of the head. This phase typically lasts from several hours to up to three days. Headache phase pain can vary from person to person and from incident to incident, with some migraine attacks causing mild pain, while others are debilitating. The pain can shift from one side of a person’s head to the other over the course of the headache, or more commonly, may begin on one side and then gradually involve the other side. Besides pain, headache phase symptoms can include nausea, inability to sleep, anxiety, and sensitivity to sound, light, and smell. Even everyday activities — like turning on the lights or participating in physical activity — can aggravate people with migraines during this phase.
4. Postdrome
Postdrome, also called the “migraine hangover,” typically occurs after the end of the headache phase. Like prodrome and aura, not every person with migraine suffers from postdrome, but it does occur in most (approximately 80%). For those that do, postdrome may not follow every migraine attack they experience, and the length of this phase can vary. Postdrome can be just as debilitating as headache, according to some people with migraine. Symptoms of postdrome include fatigue, body aches, trouble concentrating, dizziness, and sensitivity to light. Even though the headache is over, people in postdrome are still experiencing a migraine attack and can benefit from avoiding triggers that aggravate headaches, like bright lights and strong smells. Some people have reported finding relief during this phase by engaging in relaxing activities like meditation or yoga, drinking water, and avoiding stress.
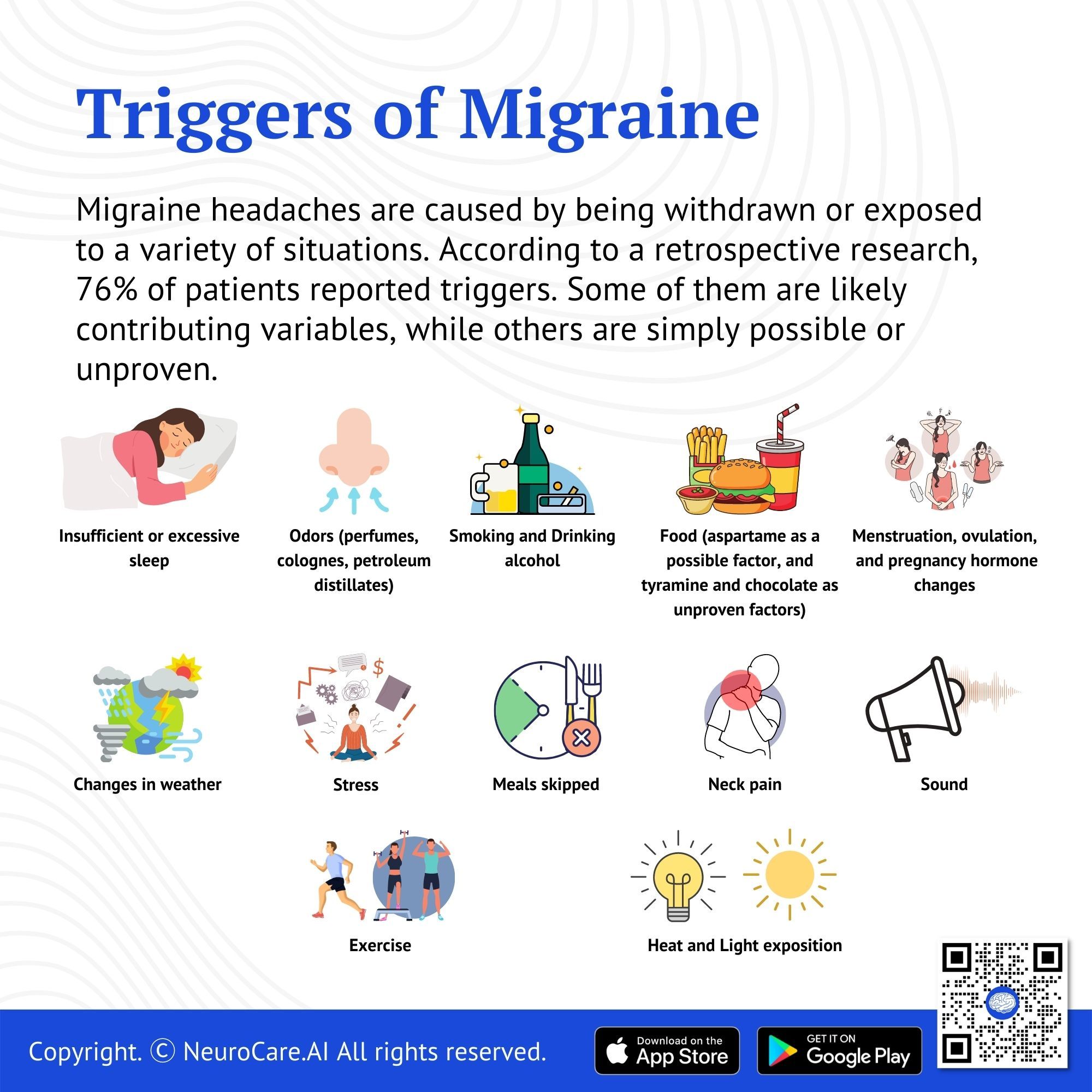
Triggers of Migraine
Migraine headaches are caused by being withdrawn or exposed to a variety of situations. According to a retrospective research, 76% of patients reported triggers. Some of them are likely contributing variables, while others are simply possible or unproven.
1. Stress
2. Menstruation, ovulation, and pregnancy hormone changes
3. Meals skipped
4. Changes in weather
5. Insufficient or excessive sleep
6. Odors (perfumes, colognes, petroleum distillates)
7. Neck pain
8. Light exposition
9. Ingestion of alcohol
10. Smoking
11. Sleeping late
12. Heat
13. Food (aspartame as a possible factor, and tyramine and chocolate as unproven factors)
14. Exercise
Types of Migraine
According to the International Headache Society's Headache Classification committee, migraine can be divided into subtypes:
Common Types of Migraines
- Migraine without aura is a recurrent headache episode that lasts 4 to 72 hours and is usually unilateral in nature, pulsing in quality, moderate to severe in severity, increased by physical activity, and accompanied by nausea and light and sound sensitivity.
- Migraine with aura is characterized by recurring, fully reversible attacks that last minutes and include one or more of the following unilateral symptoms: visual, sensory, speech and language, motor, brainstem, and retinal symptoms, which are commonly followed by headache and migraine symptoms.
Uncommon Types of Migraines
- Hemiplegic migraine is a rare type of migraine that is accompanied by temporary weakness on one side of the body. There is a similarity between these symptoms and those of a stroke. Paralysis, speech disturbances, and weakness on one side of the body are some of the symptoms associated with this condition.
- Ophthalmic migraines present with visual disturbances, blind spots, and blindness in one eye, which last about a minute before the migraine begins.
- Ophthalmoplegic migraines are common among young children and adolescents. It is characterized by severe pain behind the eye, double vision, drooping of the eyelids, vomiting, and seizures.
- Vestibular migraine is characterized by vertigo (a feeling of movement), dizziness, or problems with balance. During the attack, they may feel that the entire room is spinning, and they may feel like they are moving even when they are not.
- Basilar migraine is called such when it occurs in the basilar region of the brain. Most often, it affects adolescents and young women. Most likely, it is the result of hormonal changes in the body. It is characterized by dizziness or vertigo as well as slurred speech and loss of consciousness.
- Abdominal migraine affects four out of 100 people both as children and as adults. This condition tends to affect younger children most frequently. Aside from nausea and vomiting, a child may also experience dizziness and lightheadedness. These symptoms may last for up to three days.
Treatment
Your doctor may prescribe medication to help you cope with the pain and advise you to make certain lifestyle modifications. He may also recommend drugs to help you avoid migraines. Take your prescription migraine treatment as soon as the pain begins, rather than waiting for it to get worse. Then lie down in a dark, quiet room and cover your eyes with a cold cloth.
Pharmacological Treatment
- Acute (Abortive) treatment aims to stop a headache from getting worse. It must be treated as soon as possible and with a large single dose. In patients with migraine-induced gastric stasis, oral medications may be ineffective. As a result, parenteral medicine may be the only option for some individuals, particularly those suffering from nausea or vomiting. There are several treatment options:
- Common options for abortive therapy include:
- NSAIDs
- Triptans
- Antiemetics
- Calcitonin-gene-related peptide antagonists
- More advanced options are available for abortive therapy if the above methods fail. These options are generally instituted under direct guidance of physician:
- Ergots
- Dexamethasone
- Prophylactic treatment aims to minimize attack frequency, enhance reactivity to the severity and length of acute attacks, and reduce impairment. Before a long-term prophylactic treatment is generally initiated, we need to ensure that Individual migraine triggers were identified and the utmost measures are taken to avoid those triggers.
- The decision to start prophylactic medication is made in consultation with the treating physicians and depends on a multitude of factors; severity, frequency, impact, triggers, etc.
- The decision of choice on prophylactic medication is made in consultation with the treating physicians and depends on a multitude of factors; comorbidities, lifestyle, regimen, etc.
- Of Note, there is a multitude of prophylactic medications available and most patients go through a process of trial-and-error to find the best possible medication. Some treatment agents are the following:
- Beta-blockers
- Anti-depressants
- Anticonvulsants
- Calcium channel blockers
- Calcitonin gene-related peptide antagonists
Non-Pharmacological Treatment
- Transcutaneous supraorbital nerve stimulation can reduce intensity.
- Transcranial magnetic stimulation is an effective second-line treatment with minimal side effects. Additionally, it can be used to treat chronic migraine headaches. For people with epilepsy, this is not fully recommended.
- Non-painful remote electric neurostimulation could be considered a first-line treatment.
- Peripheral nerve blocking
- Cognitive-behavioral therapy
- Biofeedback
Prevention
In order to improve mental health, patients must change their lifestyles; however, social support is very important in order to increase patient involvement.
- Regular exercise
- Yoga
- Relaxation training
- Reduction of triggers
- Detoxification
- Butterbur
- Melatonin
To help prevent migraines, consider the following lifestyle changes:
- Alter your eating habits. Don't skip meals, but stay away from foods that can cause migraines. Because they can differ from person to person, keep a "headache journal" and record the things you ate before your migraine began. This aids in the identification of foods to avoid.
- Establish appropriate sleeping habits. Even on weekends, stick to a regular sleeping and waking routine.
- Take your medicine exactly as directed. If you're in pain, try aspirin or acetaminophen (Tylenol), unless you're allergic to these medications. If you require greater pain medicine, your doctor will prescribe it. Take it precisely as directed because some drugs can make migraines worse if taken too often.
- Lower your stress levels. Use relaxation techniques like yoga, meditation, progressive muscle relaxation, or biofeedback on a regular basis. Your healthcare professional can give you additional information about these stress relievers.
Which Lifestyle Do You Need to Consider?
Despite significant advances in understanding the pathophysiology and treatment of migraine, lifestyle modifications have become increasingly important.
Physical activity
Maintaining a physically active body, improved management of obesity, a healthy diet, and a better lifestyle, such as adequate sleep and avoiding drug abuse and alcohol, have been shown to significantly reduce attacks. For migraine sufferers, these factors need to be evaluated in their overall management strategies.
Migraines are associated with obesity and being overweight. In obese individuals, overactivation of the reward circuitry can result in food addiction and/or compulsive eating. High physical inactivity is often associated with more frequent migraines. Aerobic activity results in a similar impact as taking medication for migraine. There is no migraine-specific diet. Migraine duration and frequency decreased in people who ate a diet high in omega-3 fatty acids. Several studies have found that missing meals increases the likelihood of having a migraine.
Alcohol Intake and Smoking
Alcohol triggers migraine attacks in about 75% of patients. Migraine attacks can be triggered by smoking or nicotine use in migraine onset. Among former smokers, smoking cessation is recommended. The pathogenesis of smoking or using nicotine in migraines is controversial and affects the central nervous system.
Hydration
A headache is associated with fluid restriction and dehydration. Increased hydration status results in more balanced plasma osmolality and ion concentrations, which can help with migraine.
According to the American Migraine Foundation, caffeine can provide relief from migraine attacks. However, overconsumption of caffeine could lead to dependency and frequent migraine attacks. Caffeine should be taken less frequently or eliminated as part of a migraine treatment plan and because it is not prescribed. According to the US National Library of Medicine, caffeine intake, unlike many other unavoidable migraine triggers, is a modifiable risk factor.
Identifying and avoiding migraine attack triggers, and avoiding lifestyle factors that contribute to more frequent migraine episodes, are all part of a migraine prevention approach. It is safe and economical and poses little risk to the patient. In a recent update, the acronym SEED, which stands for Sleep, Exercise, Eat, and Diary was developed to encapsulate the lifestyle improvements related to migraine treatment. Non-pharmacological migraine treatments are proven to be beneficial in studies. Considering chronic migraine sufferers are more prone to chronic migraines than episodic migraine sufferers, regular lifestyle changes can help mitigate chronic migraine.
How can we help?
In order to help people with migraine thrive at work, the following 10 reasonable adjustments are most commonly used to assist them:
- Offer them flexible working hours and breaks.
- Give them enough time to attend to their medical appointments.
- Make changes for them and adjust the overhead lighting.
- Use technology that is migraine-friendly such as an anti-glare screen.
- Offer flexible work-from-home policies specifics for migraine victims.
- Modify their workstation so they can work efficiently (desk height, the inclination of chairs, etc).
- Give them 100% access to drinking water.
- Ensure quietness in the entire workplace.
Consult your Doctor
Because no test can identify migraines, your doctor will ask you questions about your symptoms and do an examination. He might request tests like X-rays and scans to rule out alternative possibilities for your headaches. He'll establish the diagnosis based on your symptoms if no other cause is uncovered.
Remember that to avoid migraines, it is important to practice good self-care and avoid triggers at the same time. Once a migraine has started, it is of utmost importance to begin early treatment with migraine-specific medication as soon as possible.
You should immediately call 911 or go to the nearest emergency department if your migraine symptoms become more severe than normal. This is especially true if you experience symptoms such as confusion, fever, difficulty speaking, or arm weakness.
DISCLAIMER:
The information in this document is for general educational purposes only. It is not intended to substitute for personalized medical professional advice. NeuroCare.AI makes every effort to provide accurate and timely information, but makes no guarantee in this regard and disclaims responsibility for adverse consequences resulting from its use. For further information, consult a physician and the organization referred to herein.
AizaMD™: Revolutionizing Clinical Documentation
Discover the power of our ambient clinical documentation system, designed to transform clinical encounters into structured SOAP notes with unmatched ease. Experience exceptional value for less than $3 per day—cheaper than your daily coffee!
- Save Time: Free up over 90 minutes daily for each provider.
- Boost Revenue: Increase daily revenue by at least $1,000 per provider.
- Enhance Coding Quality: Our detailed documentation supports superior coding accuracy, ensuring optimal reimbursement.
- Maximize Engagement and Interaction: Dedicate more time to patient care and less to typing, fostering richer and more effective conversations between clinicians and patients
AizaMD™: Automated Radiology Report Generation!
Discover our breakthrough Radiology AI reporting platform built on Ambient AI. It enhances productivity and minimizes fatigue. Benefit from best-in-class accuracy with our automated radiology report generation, all at market-leading pricing.
📈 Efficiency: Cut dictation times by up to 50% (Less words, More report!
🎯 Focus: Keep your eyes on the images, not the keyboard!
💸 Revenue: Boost revenue by at least 20%
📑 Clarity: Patient summary in plain English