Slug
headache-basics
Video
Category
Headache
Excerpt
Headaches can develop gradually or suddenly, last less than a minute or last a few days. A headache disorder is characterized by head, neck, and shoulder discomfort. Throughout this article, we will discuss headaches as well as all the other factors that provide a basic understanding of headache disorders.
Authors
Tags
Featured
Featured
Ready to Publish
Ready to Publish
Publish Date
Sep 5, 2022
Introduction
The term headache refers to a pain in the head. These symptoms may be localized or may radiate throughout or portions of the head. There are times when headaches are accompanied by neck and shoulder pain.
A headache is characterized by these characteristics:
- severe pain in the head or neck region
- throbbing/pulsating sensation
- dull discomfort
Headaches can develop gradually or unexpectedly and may last from less than a minute to several days. Most people suffer from headaches at some point in their lives. If severe, they can affect a person's quality of life and diminish their productivity at work and in school. Most headaches can be treated with medications and/or lifestyle changes. If you are experiencing headache symptoms, your healthcare provider is available to evaluate your symptoms and provide you with strategies to relieve them.

💡 Key Facts:
- Up to 75% of the adults experience headaches; with a lifelong prevalence of 96%, mostly among females.
- Most headaches are a result of benign conditions.
- A pain localized anywhere in the head or radiating from neck or shoulder region..
- Often treatable with the use of over-the-counter drugs.
- Nearly half of the adult population has had a headache at least once in the last year.
- Recurrent headache disorders are associated with significant personal and societal burdens of pain, disability, poor quality of life, and financial costs.
- Health care providers diagnose headache disorders improperly in only a minority of cases worldwide.
- In the world, headache is underestimated, under-recognized, and under-treated.
- There is a need to investigate it thoroughly as, sometimes, it can indicate the beginning of a potentially serious condition.
- A report by the World Health Organization features headaches as one of the top 10 causes of disability. The number one complaint of women is headaches, which are considered comparable to arthritis and diabetes, and worse than asthma.
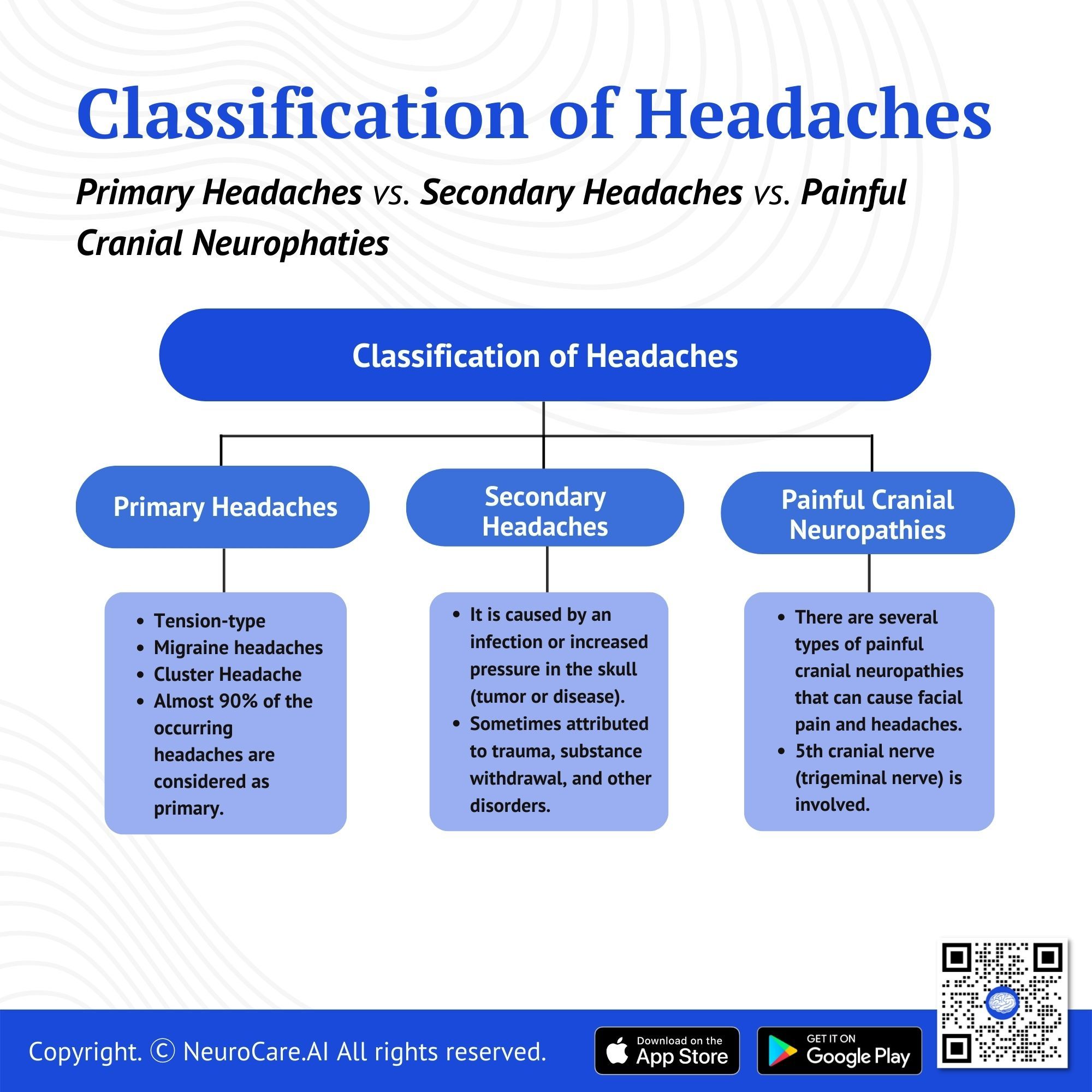
Classification of headaches: Primary headaches vs. secondary headaches vs. painful cranial neuropathies
- Primary Headaches - are not only limited to tension-type, trigeminal autonomic cephalgia, and migraine headaches but almost 90% of the occurring headaches are considered primary.
- Secondary Headaches - are caused by another medical problem like an infection or increased pressure in the skull caused by a tumor or disease. It accounts for fewer than 10% of all headaches. These are sometimes attributed to trauma to the head and neck, cranial and cervical valvular disease, a substance withdrawal, disorder to the homeostasis, or disorder to the facial and cervical structures (eyes, neck, nose, sinuses, teeth, cranium, mouth), and psychiatric disorder.
- Painful Cranial Neuropathies - The cranial nerve can be related to several different types of painful facial and headache disorders. Current research indicates that the fifth cranial nerve, also known as the trigeminal nerve, underlies many of the known headache and facial pain conditions.
What are the different types of Primary Headaches?
Headache is among the most common disorders of the nervous system. The two most common types of headaches are tension headaches, migraine headaches, and chronic headaches. In terms of symptoms and treatment, tension headaches and migraine headaches are frequently interchangeable. Relief methods and triggering factors can differ from person to person.
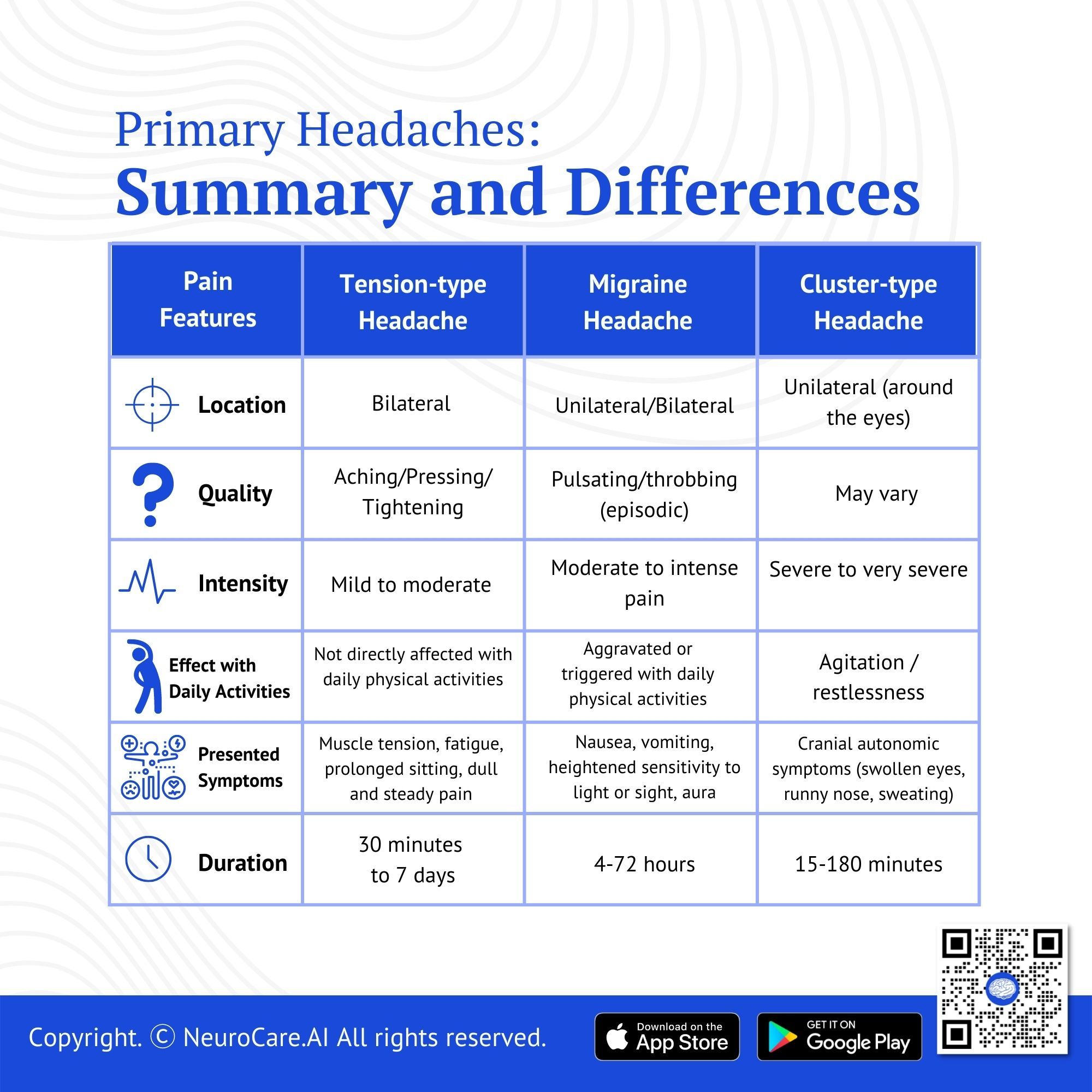
Pain Features | Tension-type Headache | Migraine Headache | Cluster Headache |
Location | Bilateral | Unilateral/Bilateral | Unilateral (around the eyes) |
Quality | Aching/Pressing/
Tightening | Pulsating/throbbing (episodic) | May vary |
Intensity | Mild to moderate | Moderate to intense pain | Severe to very severe |
Effect with Daily Activities | Not directly affected by daily physical activities | Aggravated or triggered by daily physical activities | Agitation / restlessness |
Presented Symptoms | Muscle tension, fatigue, prolonged sitting, dull and steady pain | Nausea, vomiting, heightened sensitivity to light or sight, aura | Cranial autonomic symptoms (swollen eyes, runny nose, sweating) |
Duration | 30 minutes to 7 days | 4-72 hours | 15-180 minutes |
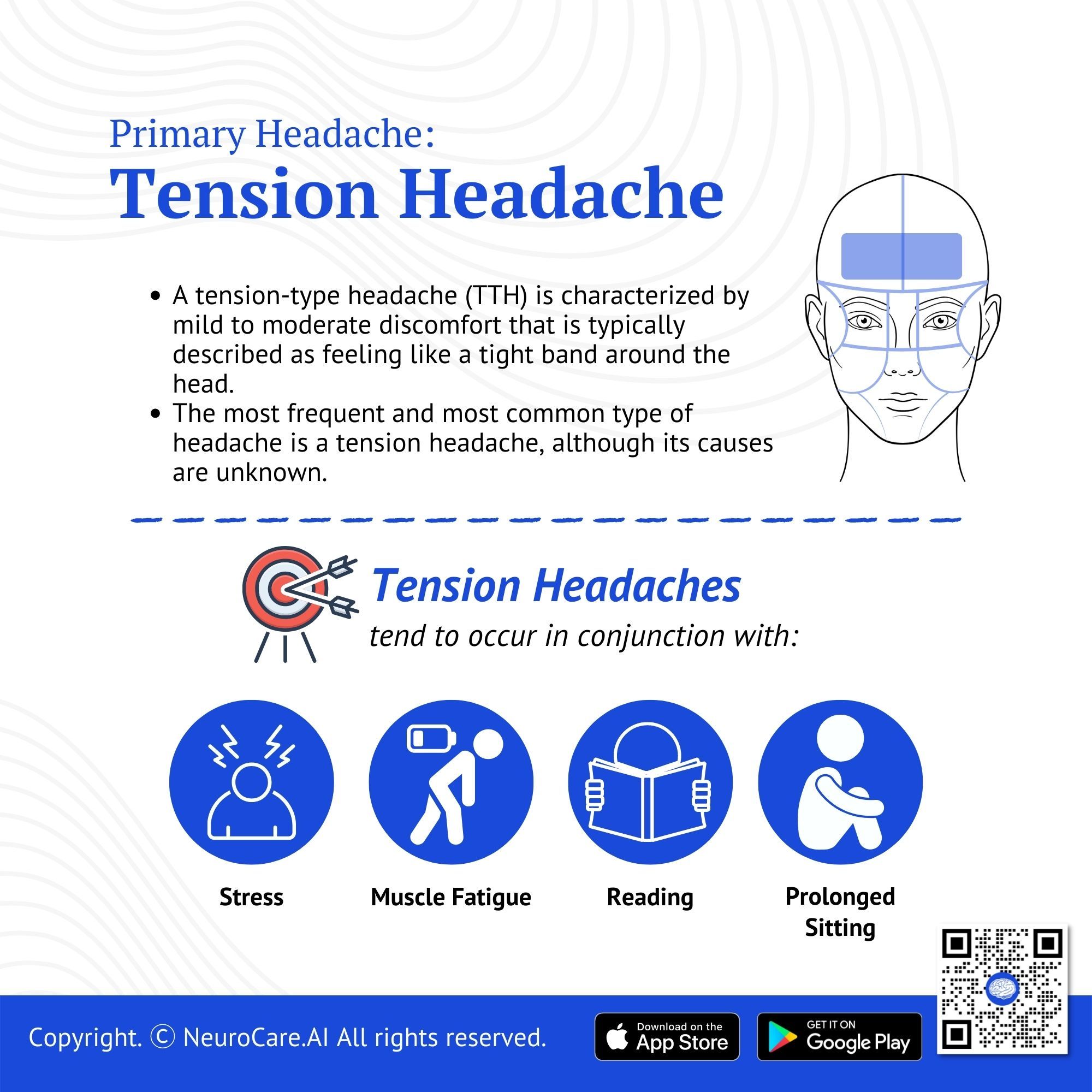
Tension Headache
A tension-type headache (TTH) is characterized by mild to moderate discomfort that is typically described as feeling like a tight band around. The most frequent and most common type of headache is a tension headache, although its causes are unknown.
Tension headaches tend to occur in conjunction with stress, fatigue, or muscle strain. Tension headaches can be triggered by activities that place the head and neck in a tense, prolonged position (e.g. reading, keyboarding, chewing gum, or grinding teeth).
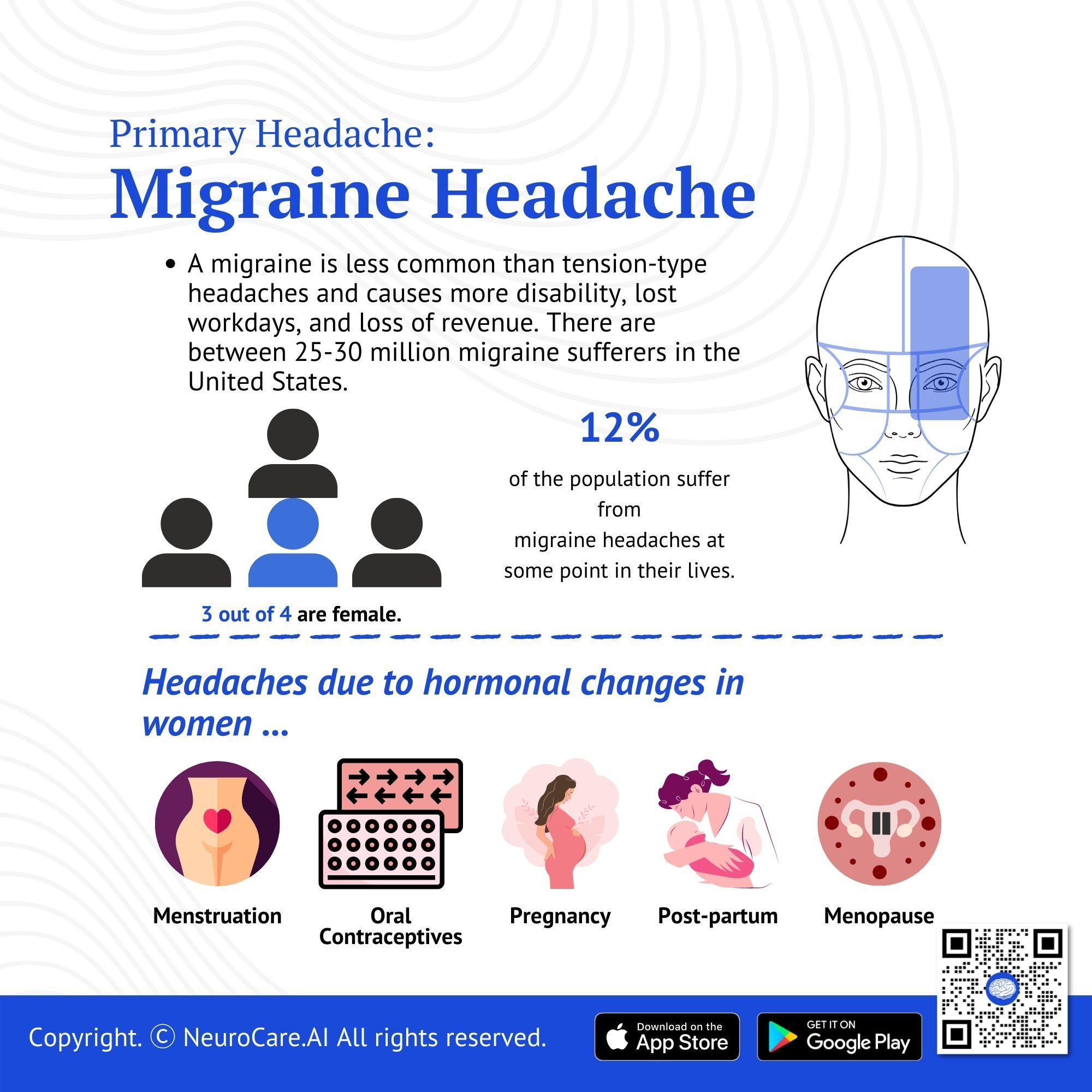
Migraine Headache
A migraine is less common than tension-type headaches and causes more disability, lost workdays, and loss of revenue. There are between 25-30 million migraine sufferers in the United States.
- There are about 12% of the population (about 6% of men and 18% of women) who suffer from migraine headaches at some point in their lives.
- Most migraine sufferers are female, with 3 out of 4 being female.
- Hormonal changes often cause migraines in women who are menstruating, taking oral contraceptives, pregnant, postpartum, and going through menopause. When you are using oral contraceptives, you should inform your clinician if headaches increase in frequency or intensity. Some headaches may be reduced by switching to a different oral contraceptive pill. There are times when it is necessary to stop taking a hormone treatment or pill.
The incidence of migraine headaches among women is three times greater than that among men. In about 70 to 80% of cases, migraine sufferers have a family history of the condition.
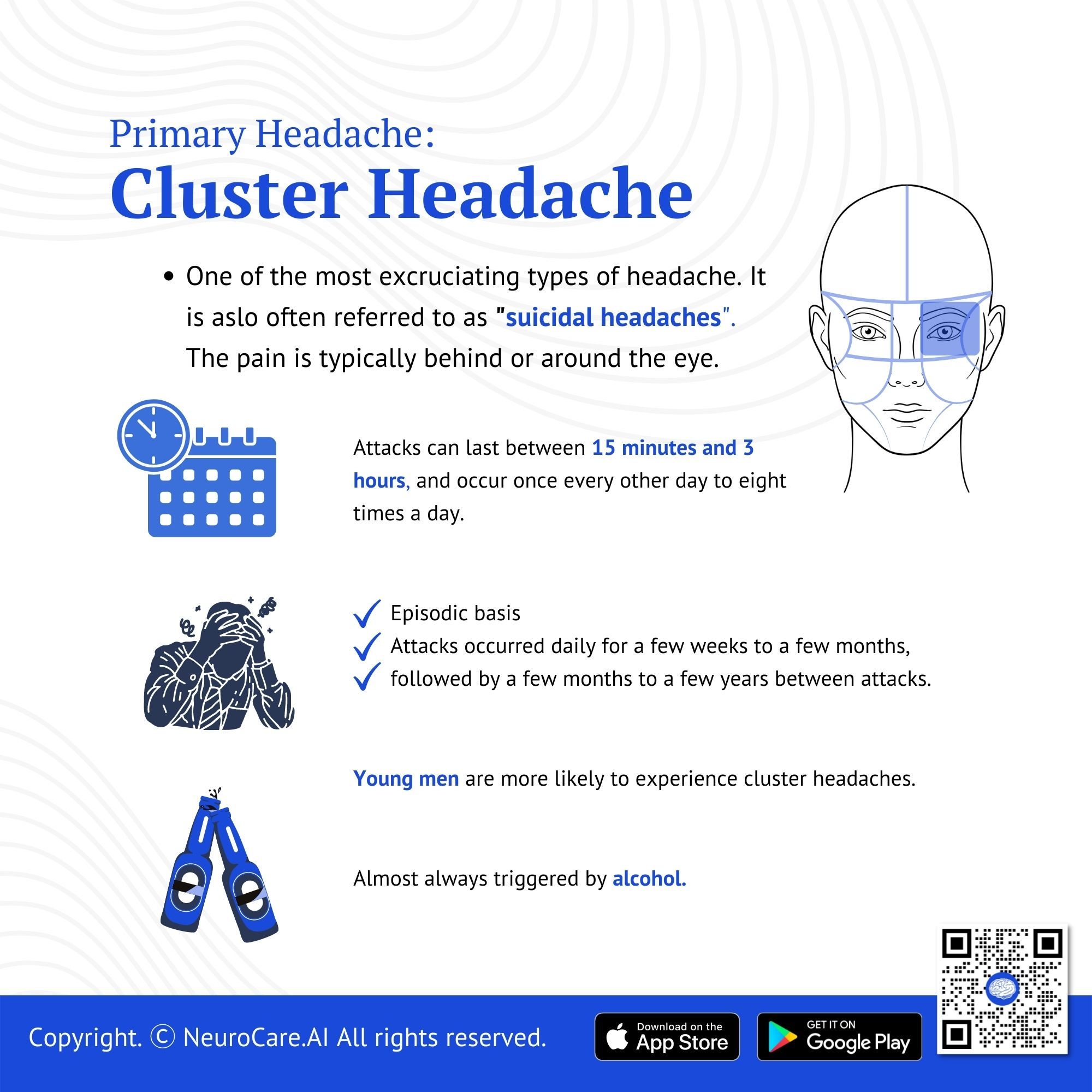
Cluster Headache
One of the most excruciating types of headache is a cluster headache. This type of headache occurs in cyclical patterns or clusters. Typically, cluster headaches wake you up in the middle of the night with tremendous pain around one of your eyes. Sometimes, headache clusters are followed by remission periods in which headaches cease. For months or even years after remission, there are no headaches. Fortunately, cluster headaches are rare and not fatal. Cluster headache attacks can be reduced in intensity and duration with treatment. In addition, drugs can reduce the frequency of cluster headache attacks.
- Young men are more likely to experience cluster headaches, and the pain is excruciating, often referred to as 'suicidal headaches'.
- Attacks can last between 15 minutes and 3 hours, and occur once every other day to eight times a day.
- There is a great deal of restlessness and agitation, and the patient often sweats excessively.
- There is striking circadian rhythmicity with attacks occurring at the same time every day.
- Almost always, an attack is triggered by alcohol.
Most cluster headaches occur on an episodic basis, with attacks occurring daily for a few weeks to a few months, followed by a few months to a few years between attacks. An individual suffering from chronic asthma has continual attacks for a year or longer without remission periods that last longer than a month.
🧠 Insights: The vast majority of headache disorders are primary headache disorders, with migraine and tension-type headaches (TTH) being the most common. There are 60–80% of people affected by TTH, whereas 15% of people suffer from migraine (male 7.6%, female 18.3%). It is uncommon to have cluster headaches (0.1%), but they are frequently misdiagnosed and mistreated. Medication overuse headache (MOH) is a secondary headache disorder that often occurs in conjunction with primary headache disorders and is usually diagnosed with them.

Headache Triggers
- A strong surge of stress and emotion
- Sleep deprivation/ oversleeping
- Bright, flashing lights
- Eyestrain
- Low blood sugar
- Caffeine
- Changes in weather
- Food triggers such as peanuts, MSG, aspartame
.jpg)
Pharmacological treatment for headaches
Treatment for headaches is divided into two medication regimens:
- Abortive medications. Studies have been conducted on anti-inflammatory drugs and simple analgesics for treating headaches, using headache attacks as models for acute pain. According to the International Headache Society, NSAIDs are the first-line drugs used in headache research.
- Prophylactic medications. It is possible to require daily prophylaxis medication for chronic headache sufferers. The choice and necessity of prophylaxis medication should always be discussed with your physician.
Non-pharmacological treatments
Drinking extra water is a good place to start. You may be dehydrated and need to drink more water. You should also examine how much sleep you get. Sleep deprivation can result in tension headaches, so get plenty of rest. Also, don't skip any meals because hunger might cause headaches.
Your doctor can also recommend the following ways to keep you going:
- Stress management classes for stress coping techniques.
- Biofeedback. A special type of stress management technique.
- Cognitive-behavioral therapy (CBT). A type of talk therapy that enables you to sort out your emotions and eventually identify that one experience that causes the triggers.
- Acupuncture. An alternative way to release stress through the use of fine needles to a specific part of the body.
You can also apply these alternative ways to ease your tension headache:
- Apply a heating or ice pad to your head for 10-15 minutes.
- Taking a hot or cold shower can also ease the headache.
- Take in between breaks to prevent eye strain and improve your posture.
Prevention
As headaches are frequently induced by specific triggers, understanding the variables that cause your headaches is one method of preventing future occurrences.
You can keep a headache diary journal with you to help you figure out what triggers your tension headache. You can record your daily intake of nutrients (meals), daily physical activities, and anything life situation that triggers stress. Make a note of every day when you get a tension headache. You might be able to connect after a few weeks or months. For example, if your journal reveals that you had headaches on days when you ate a specific food, that food could be your trigger.
You may be able to prevent cluster headaches by avoiding the following:
- alcohol
- tobacco
- cocaine
- high altitudes
- strenuous activities
- hot weather
- hot baths
- foods that contain large amounts of nitrates, such as bacon, hot dogs, and preserved meats

When to see a doctor
Consult your doctor if tension-type headaches are interfering with your life or if you need to take headache medicine more than twice a week.
Always consult your doctor if the pattern changes or your headaches feel different than usual. Headaches can occasionally signify a dangerous medical problem, such as a brain tumor or the rupture of a weakened blood artery or aneurysm.
Should any of the following change suddenly or worsen, seek emergency treatment as soon as possible:
- high fever
- headache accompanied with a fever, stiff neck, lightheadedness, sudden seizures due to high-temperature fever, blurry or double vision, weakness and numbness, and/or mumbling/speaking difficulties
- headache worsens after a traumatic head injury
DISCLAIMER:
The information in this document is for general educational purposes only. It is not intended to substitute for personalized medical professional advice. NeuroCare.AI makes every effort to provide accurate and timely information, but makes no guarantee in this regard and disclaims responsibility for adverse consequences resulting from its use. For further information, consult a physician and the organization referred to herein.
AizaMD™: Revolutionizing Clinical Documentation
Discover the power of our ambient clinical documentation system, designed to transform clinical encounters into structured SOAP notes with unmatched ease. Experience exceptional value for less than $3 per day—cheaper than your daily coffee!
- Save Time: Free up over 90 minutes daily for each provider.
- Boost Revenue: Increase daily revenue by at least $1,000 per provider.
- Enhance Coding Quality: Our detailed documentation supports superior coding accuracy, ensuring optimal reimbursement.
- Maximize Engagement and Interaction: Dedicate more time to patient care and less to typing, fostering richer and more effective conversations between clinicians and patients
AizaMD™: Automated Radiology Report Generation!
Discover our breakthrough Radiology AI reporting platform built on Ambient AI. It enhances productivity and minimizes fatigue. Benefit from best-in-class accuracy with our automated radiology report generation, all at market-leading pricing.
📈 Efficiency: Cut dictation times by up to 50% (Less words, More report!
🎯 Focus: Keep your eyes on the images, not the keyboard!
💸 Revenue: Boost revenue by at least 20%
📑 Clarity: Patient summary in plain English