Slug
epilepsy-advanced
Video
Category
Epilepsy
Excerpt
Epilepsy is a neurological brain disorder characterized by abnormal brain activity. Mind-related symptoms include convulsions, loss of consciousness, and convulsions caused by this condition. Throughout this article, we will discuss the aspects of understanding epilepsy.
Authors
Tags
Featured
Featured
Ready to Publish
Ready to Publish
Publish Date
Aug 15, 2022
Introduction
Epilepsy is a neurological brain disorder in which clusters of neurons in the brain fire signals abnormally. It affects the mind that causes odd sensations, behavior, convulsions, and loss of consciousness. It is also known as a common serious brain disorder characterized by recurrent epileptic seizures.
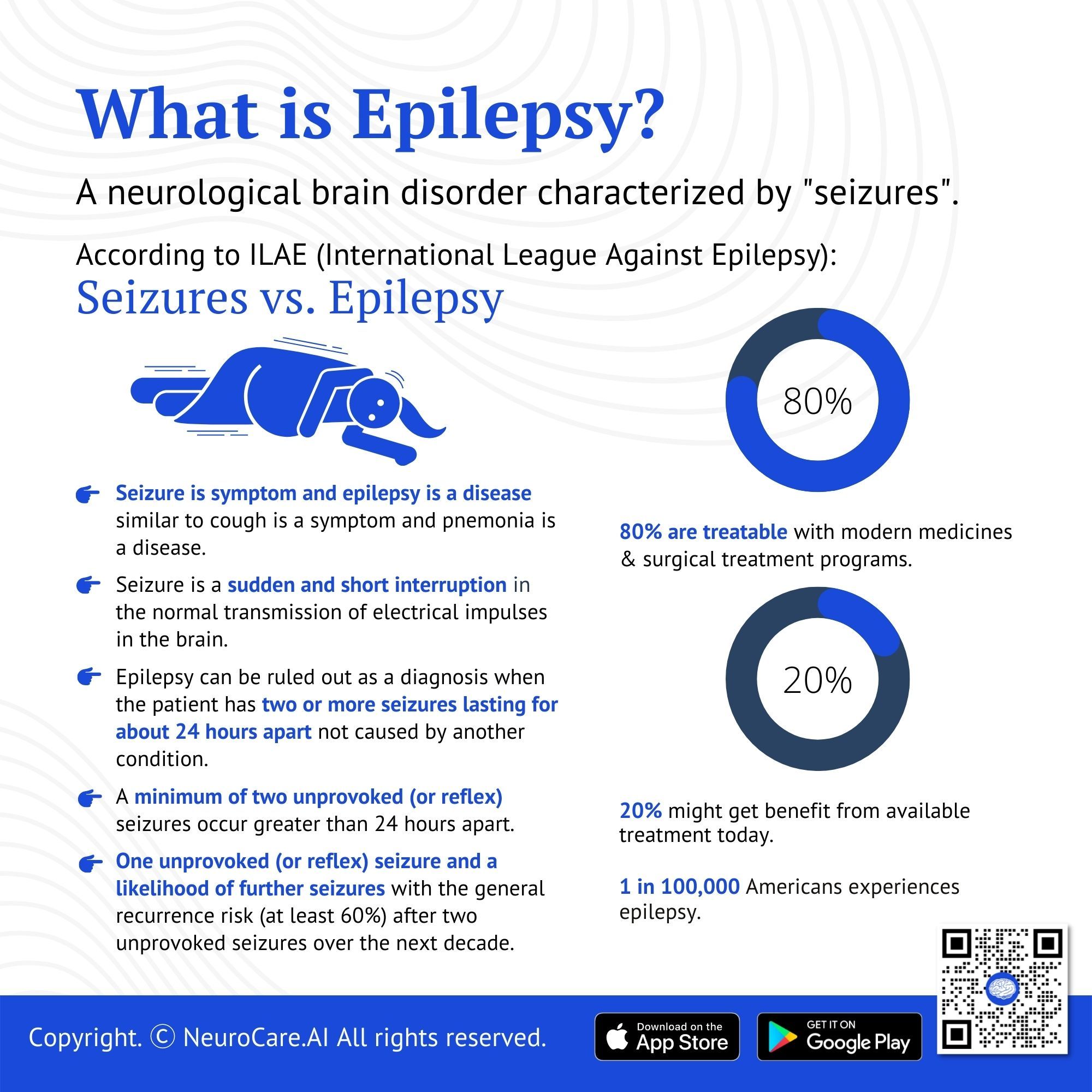
There is a 1 in 100,000 population ratio in America that experiences epilepsy. About 80% percent of those patients diagnosed with epilepsy are known to be treatable with modern medicine and surgical techniques treatment programs. The remaining 20% of people with epilepsy may even directly benefit from the best available treatment today.
Seizure vs epilepsy
Seizure is a symptom and epilepsy is a disease similar to cough is a symptom and pneumonia is a disease. A seizure can happen due to multiple reasons including not limited to alcohol withdrawal and drug use. People who have their first seizure are much more likely to have a second one, so doctors want to know what the cause of the seizure is.
- A seizure is when there is an abnormal excessive or synchronous brain activity that results in a transitory occurrence of symptoms or signs. This can cause unusual behaviors, body movements, and sensations. It can cause a person to lose consciousness, convulse, fall, stay still for a period of time (staring spell), or turn pale.
- Epilepsy has considered if the patient fulfills any of the following criteria:
- A minimum of two unprovoked (or reflex) seizures occur greater than 24 hours apart.
- One unprovoked (or reflex) seizure and a likelihood of further seizures with the general recurrence risk (at least 60%) after two unprovoked seizures over the next decade.
- Diagnosis of an epilepsy syndrome
- Sometimes, regardless of what caused the seizure, you will be diagnosed with epilepsy. If a person has two or more seizures lasting for about 24 hours apart but doesn’t have epilepsy (that is, no brain problems), he could get bad news about something else.
.jpg)
What causes epilepsy to occur?
The brain functions best when neurons interact at the proper level of excitation. Anything that upsets this balance, such as a change in the levels of neurotransmitters, can disrupt neural activity and lead to seizures. GABA (gamma-aminobutyric acid) and glutamate, two of the most studied neurotransmitters that play a role in epilepsy, are inhibitory and excitatory neurotransmitters, respectively. Research on these compounds led to drugs such as GABA and glutamate that alter the amount of chemicals or their response to signals in the brain. These treatments are known to be effective in reducing seizures.
Studies have reported that as epileptic seizures occur, there is an abnormally high level of excitatory neurotransmitters in the brain, causing a persistent barrage of excitation that disrupts normal neuronal activity. This can cause seizures-small events or disturbances in brain activity. In a small percentage of patients, the seizures are so frequent and severe that it may be necessary to try medications to reduce their frequency or severity.
Signs and symptoms of epileptic seizures
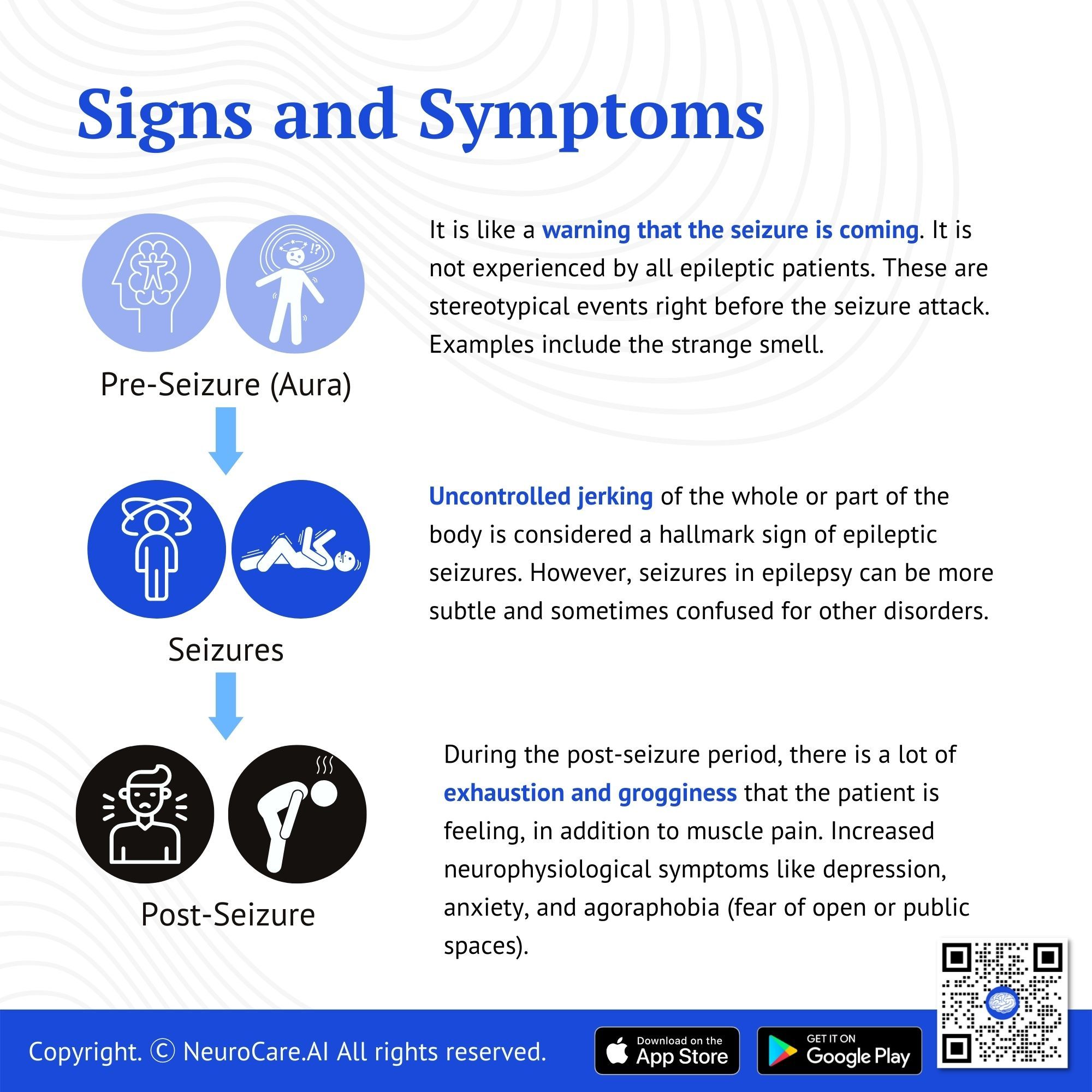
Aura (Pre-seizure) - An aura can precede a seizure attack. It is like a warning that the seizure is coming. It is not experienced by all epileptic patients. These are stereotypical events right before the seizure attack. Examples include the strange smell.
Seizures - Uncontrolled jerking of the whole or part of the body is considered a hallmark sign of epileptic seizures. However, seizures in epilepsy can be more subtle and sometimes confused for other disorders. Patients of epilepsy can suffer from:
- Seizure with Loss of awareness: This could be brief and limited to just a few seconds to complete loss of consciousness. The complete loss of consciousness can be accompanied by tongue biting, urinary leakage, etc.
- Seizures without loss of awareness: In these repetitive motor movements generally not the whole but part of the body is affected and patients do not lose awareness.
Post-seizure - The patient does experience a lot of exhaustion, grogginess, and in times of convulsive seizures, muscle pain is noted as well.
Other Symptoms - Patients with epilepsy do have an increase in neurophysiological symptoms like depression, anxiety, and agoraphobia (fear of open or public places). Patients experiencing high intensity and frequency of seizures may develop cognitive disabilities.
_Edited_Square_Video.jpg)
What are the different kinds of seizures?
Although the term “epilepsy” technically refers to any disorder that includes these sudden attacks, in common usage, it refers to disorders characterized by having multiple unprovoked seizures. The symptoms of an epileptic episode will usually be the same from episode to episode, since epileptic seizures tend to be the same type. Doctors generally classify seizures as either focal or generalized, based on how and where the abnormal brain activity begins.
The hemisphere of the brain which is involved will determine which side of the body the seizure affects.
Focal Seizure
Focal seizure is the most common form of epilepsy. The seizures remain localized to one hemisphere of the brain and do not involve both hemispheres. Focal or partial, seizures only seem to affect one hemisphere of the brain. These seizures include jerking movements or other sensations on only one side of the body.
It is further categorized as retained awareness or impaired awareness. Another category used includes the presence or absence of motor symptoms. If the awareness is not applicable focal seizure can be categorized according to the presence or absence of motor symptoms.
.jpg)
Generalized Seizure
Generalized epilepsy affects the brain bilaterally (meaning, it affects both sides of the brain). Symptoms typically don’t come on during sleep and can occur any time during the day (during any activity). More than 50% of people with epilepsy experience this type of epilepsy. It is further categorized as motor onset or non-motor (absence) seizures.
Motor Seizures
- Tonic-Clonic Seizures - In a typical tonic-clonic seizure, the person loses consciousness, stiffens, and falls to the floor. Breathing stops for about a minute and may be followed by repeated jerking movements of the arms and legs (tonic phase) and then the entire body (clonic phase). This is sometimes referred to as “grand mal seizures.”
- Tonic Seizures - Tonic seizures typically cause stiffening of body muscles, generally those in the back, legs, and arms. This may be accompanied by opening the eyes widely and staring, and afterward, some people are dazed for a short period.
- Myoclonic Seizures - Myoclonic seizures are seizures that cause jerks or twitches of the upper body, arms, or legs. If a person has a sudden jerk or twitch, they may be able to feel it, but they have no control over it. The seizure may stop after a few seconds or eventually spread throughout the whole body.
- Atonic Seizures - are the result of a sudden loss of muscle tone. This type of seizure causes a sudden loss of muscle tone, leading to a fall or nod off, sometimes without warning. Because atonic seizures disrupt activities without impairing consciousness, most people have no memory of the event.
Non-Motor (Absence) Seizure
A brief seizure with no loss of consciousness during which a person may appear to be staring into space (epileptic stare). The person may have jerking or twitching muscles and lose control of urine or stool (incontinence). It is sometimes referred to as a petit mal seizure. They are further classified as :
- Typical
- Atypical
- Myoclonic
- Eyelid myoclonia
Secondarily generalized seizures
These are usually partial seizures evolving into generalized seizures, most often with tonic-clonic convulsions. Although secondary or "secondarily generalized" seizures are similar to the first one, they don't tend to have any distinctive features.
Unknown Seizure
If the beginning of a seizure is not known, it’s called an “unknown onset seizure.” While sometimes people may feel that a seizure is going to happen, sometimes people can have seizures without having an aura or warning about one, so if it’s not witnessed or seen by anyone, the doctor may describe it as an unknown onset seizure. This can happen when seizures happen at night, in someone who lives alone, or if observers are too distracted to notice the patient.
Epilepsy diagnostic investigation
Doctors and researchers have developed several tests to help diagnose epilepsy. They normally the combination of the following different types of investigations:
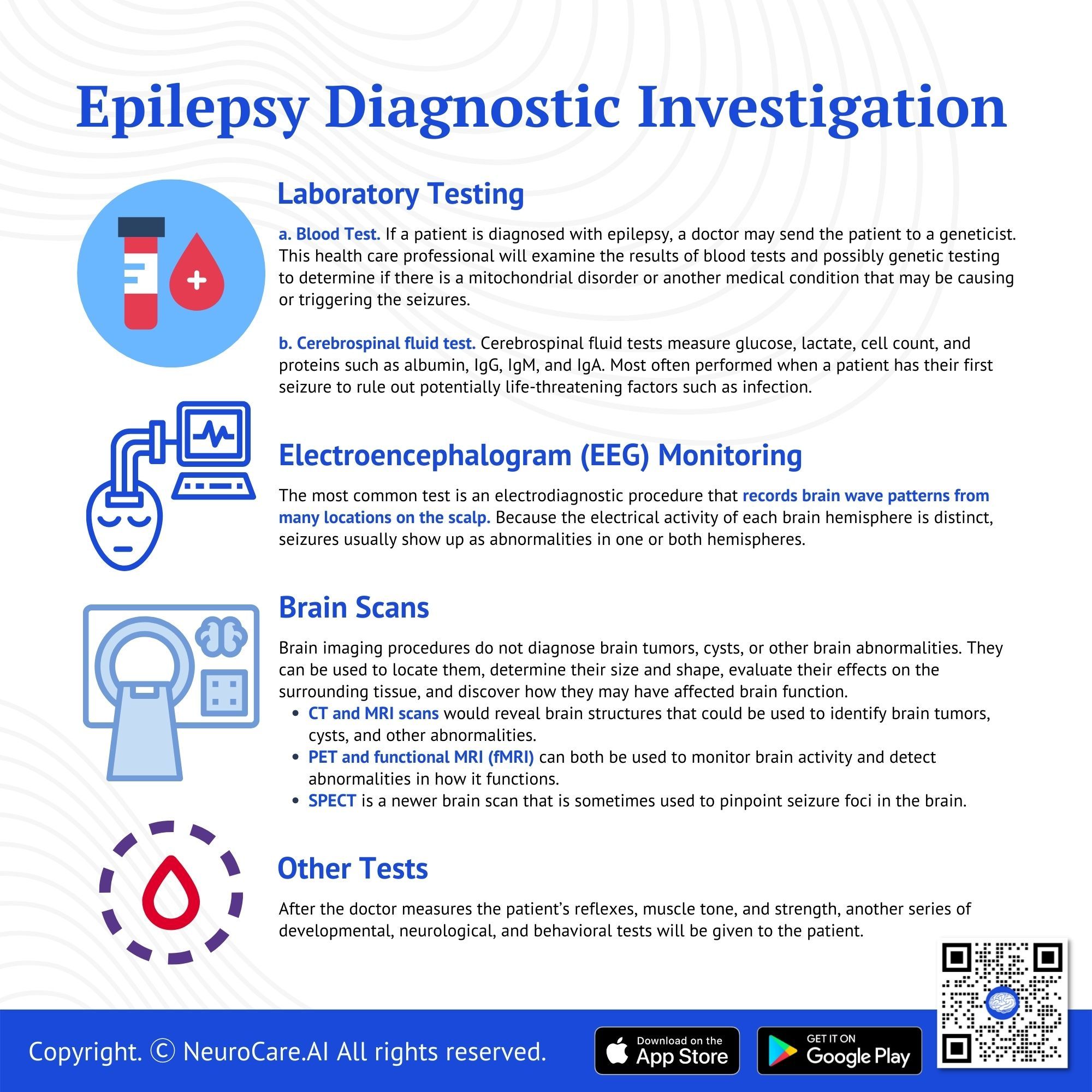
Laboratory Testing:
- Blood Tests. If a patient is diagnosed with epilepsy, a doctor may send the patient to a geneticist. This health care professional will examine the results of blood tests and possibly genetic testing to determine if there is a mitochondrial disorder or another medical condition that may be causing or triggering the seizures.
- Cerebrospinal Fluid Tests. Cerebrospinal fluid tests measure glucose, lactate, cell count, and proteins such as albumin, IgG, IgM, and IgA. Most often performed when a patient has their first seizure to rule out potentially life-threatening factors such as infection.
- Leukocyte counts in CSF rarely rise on the first day of seizure, whereas lactate levels are raised during the first three days and are dependent upon seizure duration.
- About 34% of patients also have elevated protein levels.
Electroencephalogram is the most common test, an electrodiagnostic procedure that records brain wave patterns from many locations on the scalp. Because the electrical activity of each brain hemisphere is distinct, seizures usually show up as abnormalities in one or both hemispheres. For this reason, whenever possible, a patient’s first EEG should be performed within 24 hours of the first seizure.
Brain Scans. Brain imaging procedures do not diagnose brain tumors, cysts, or other brain abnormalities. They can be used to locate them, determine their size and shape, evaluate their effects on the surrounding tissue, and discover how they may have affected brain function. Common MRI, CT, PET, and SPECT scans are used to detect abnormalities in regions of the brain.
- CT and MRI scans would reveal brain structures that could be used to identify brain tumors, cysts, and other abnormalities.
- PET and functional MRI (fMRI) can both be used to monitor brain activity and detect abnormalities in how it functions.
- SPECT (single-photon emission computed tomography) is a newer brain scan that is sometimes used to pinpoint seizure foci in the brain.
Other Tests. After the doctor measures the patient’s reflexes, muscle tone, and strength, another series of developmental, neurological, and behavioral tests will be given to the patient. The test results may help determine if epilepsy is a factor in your symptoms in some cases. Or the doctor might perform specialized tests to help make that determination.
Epilepsy treatment
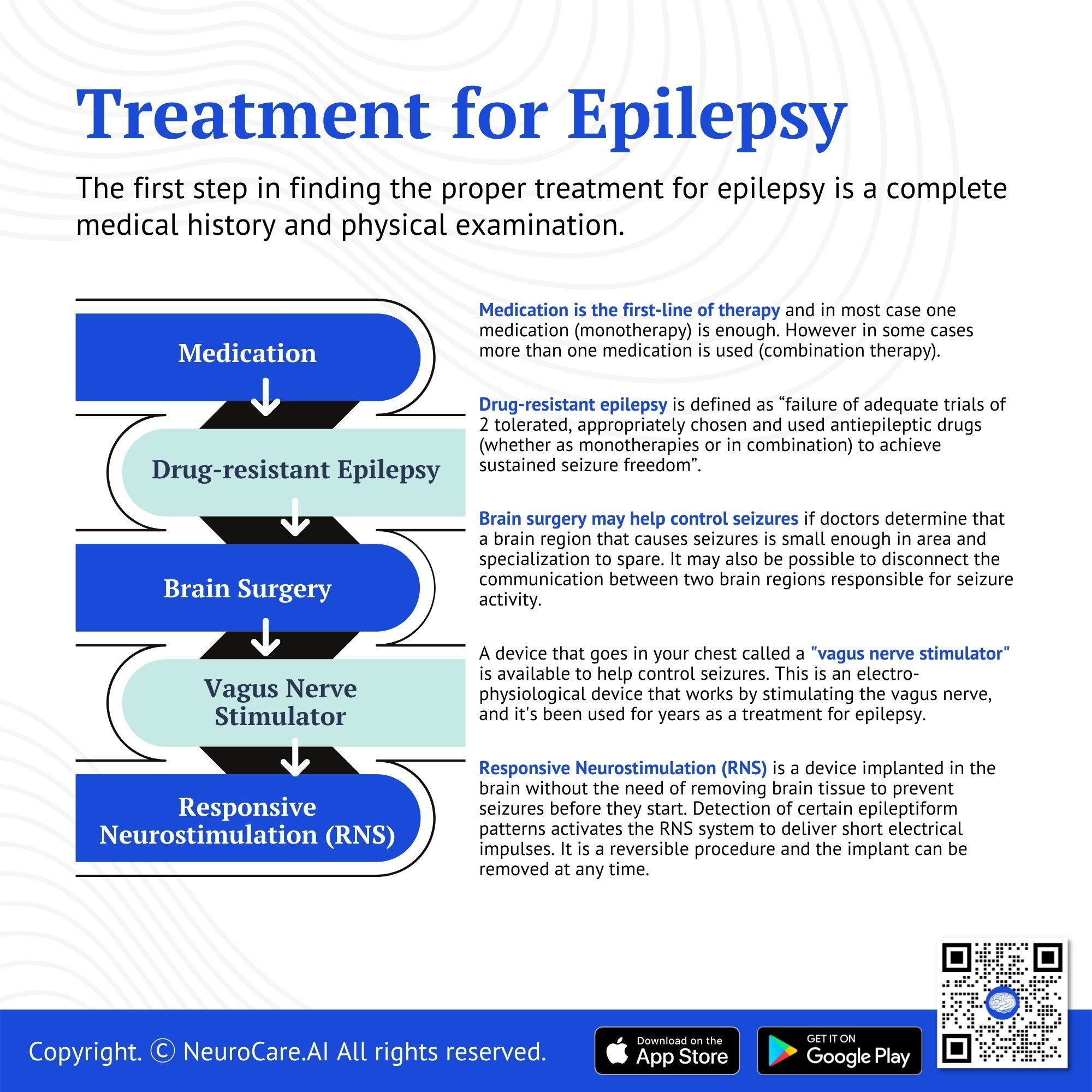
The first step in finding the proper treatment for epilepsy is a complete medical history and physical examination. For some people with epilepsy, taking medications does not control seizure activity. Many of these people have intractable epilepsy and need alternative therapies. Brain surgery is a proven treatment for intractable epilepsy, but only if performed by a neurosurgeon adequately trained and experienced in this type of surgery.
Medication (Drugs). The first effective drug for treating epilepsy was bromide, an anti-seizure medication introduced in 1857 by an English physician. More than 20 different antiepileptic drugs are available with other benefits and side effects. Your doctor will prescribe the best drug for you based on factors including your type of seizure(s), your lifestyle and age, how frequently you have attacks, and the likelihood of becoming pregnant for a woman.
- For newly developed epilepsy - a doctor may often prescribe carbamazepine, valproate, lamotrigine, oxcarbazepine, or phenytoin.
- For the Absence of Seizures - ethosuximide is known as the primary treatment. Other absence seizure treatment drugs include clonazepam, phenobarbital, and primidone.
- The drug diazepam (available as a gel) can be administered rectally by a family member for people with stereotyped recurrent severe seizures.
Monotherapy is where only one epilepsy drug is used to control seizures. This can be a good choice for most people with epilepsy. However, using one medication does not work for every person with epilepsy. Some patients have more than one type of seizure and need more than just one medicine. For these people, combination therapy may help control their seizures and reduce the side effects of the medication.
Drug-resistant epilepsy. In some case medication do not adequately control seizure. this is called Drug-resistant epilepsy and is defined as “failure of adequate trials of 2 tolerated, appropriately chosen and used antiepileptic drugs (whether as monotherapies or in combination) to achieve sustained seizure freedom”. In these cases, advanced invasive therapies are needed with a combination of medications. These advanced therapies are alone provided at highly specialized epilepsy centers designated as Level 4 by the National Association of Epilepsy Center (NAEC). These therapies include:
Brain Surgery. For most people who seek treatment for epilepsy, drugs are the first choice. Some people, however, may not be able to take or do not respond well to drugs. In those cases, surgery is an option. Brain surgery may help control seizures if doctors determine that a brain region that causes seizures is small enough in area and specialization to spare. It may also be possible to disconnect the communication between two brain regions responsible for seizure activity. The neurosurgeon’s role is to safely, accurately, and quickly perform the neurosurgical operation to minimize the risk of injury to surrounding brain tissue and vital structures. Brain surgery for epilepsy is highly specialized and is only done in select centers with the designation.
Vagus Nerve Stimulator. A device that goes in your chest called a "vagus nerve stimulator" is available to help control seizures. This is an electro-physiological device that works by stimulating the vagus nerve, and it's been used for years as a treatment for epilepsy. The vagus nerve is the longest of all cranial nerves, and when stimulated through this implant, it can reduce the severity of epileptic seizures.
Responsive Neurostimulation (RNS). A device is implanted in the brain without the need of removing brain tissue to prevent seizures before they start. Detection of certain epileptiform patterns activates the RNS system to deliver short electrical impulses. It is a reversible procedure and the implant can be removed at any time.
Appropriate medication and dosage may take some time so it is important to record the number of seizures you have and side effects to find the best therapy for your situations
More about epilepsy
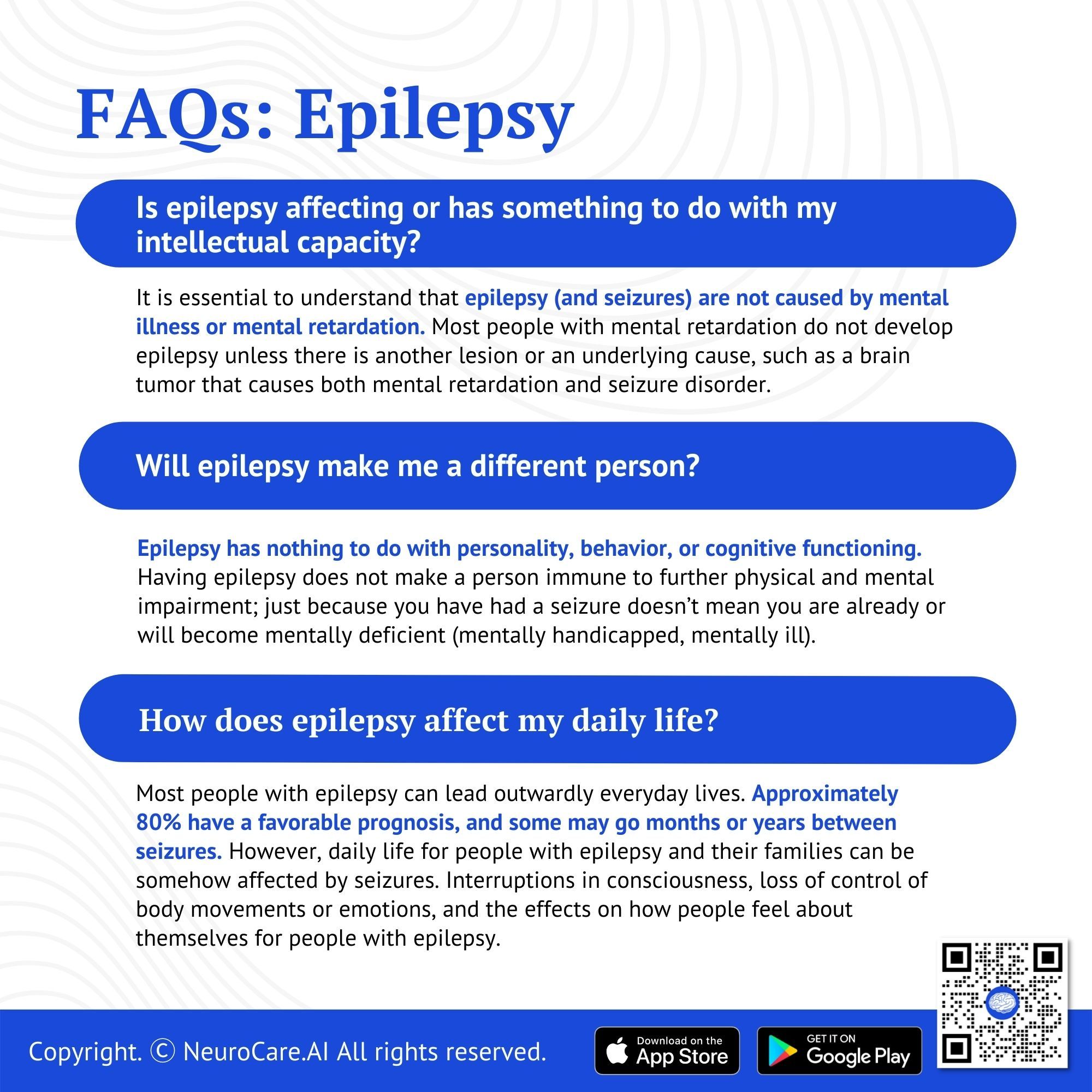
- Epilepsy on Intellectual Capacity
It is essential to understand that epilepsy (and seizures) are not caused by mental illness or mental retardation. Most people with mental retardation do not develop epilepsy unless there is another lesion or an underlying cause, such as a brain tumor that causes both mental retardation and seizure disorder.
- Epilepsy on Physical and Mental Impairment
Epilepsy has nothing to do with personality, behavior, or cognitive functioning. Having epilepsy does not make a person immune to further physical and mental impairment; just because you have had a seizure doesn’t mean you are already or will become mentally deficient (mentally handicapped, mentally ill).
- Epilepsy in Daily Life
It is normal to be curious about epilepsy. It’s a sign of caring because most people with brain disorders are stigmatized. Most people with epilepsy can lead outwardly everyday lives. Approximately 80% have a favorable prognosis, and some may go months or years between seizures. However, daily life for people with epilepsy and their families can be somehow affected by seizures. Interruptions in consciousness, loss of control of body movements or emotions, and the effects on how people feel about themselves and their abilities are some of the challenges for people with epilepsy. In addition, doctors must balance the risk of serious side effects from anticonvulsant medications against the benefits of controlling seizures. While there is no cure for epilepsy, research is uncovering important information about preventing seizures from occurring, making them less frequent or less severe, and how to increase the chances that an individual will lead a full life.
Conclusion
Living with epilepsy and seizures isn’t always easy, but it doesn’t have to stop you from living and enjoying life. People with epilepsy continue their daily routines, despite their condition. They drive to work, go out with friends or family, or enjoy hobbies they’ve always wanted. Recent medical advances have increased the availability of treatment options and better seizure control for most people with epilepsy. Research is always ongoing, and promising new insights, treatments, and even cures are being pursued—still, many unknowns, such as the exact causes of epilepsy currently under investigation. Life doesn’t have to stop when seizures do—but living well will require you and your family to learn how to manage this disorder, reduce the risks of injury, and avoid medical emergencies while taking seizure medication correctly.
DISCLAIMER:
The information in this document is for general educational purposes only. It is not intended to substitute for personalized medical professional advice. NeuroCare.AI makes every effort to provide accurate and timely information, but makes no guarantee in this regard and disclaims responsibility for adverse consequences resulting from its use. For further information, consult a physician and the organization referred to herein.
AizaMD™: Revolutionizing Clinical Documentation
Discover the power of our ambient clinical documentation system, designed to transform clinical encounters into structured SOAP notes with unmatched ease. Experience exceptional value for less than $3 per day—cheaper than your daily coffee!
- Save Time: Free up over 90 minutes daily for each provider.
- Boost Revenue: Increase daily revenue by at least $1,000 per provider.
- Enhance Coding Quality: Our detailed documentation supports superior coding accuracy, ensuring optimal reimbursement.
- Maximize Engagement and Interaction: Dedicate more time to patient care and less to typing, fostering richer and more effective conversations between clinicians and patients
AizaMD™: Automated Radiology Report Generation!
Discover our breakthrough Radiology AI reporting platform built on Ambient AI. It enhances productivity and minimizes fatigue. Benefit from best-in-class accuracy with our automated radiology report generation, all at market-leading pricing.
📈 Efficiency: Cut dictation times by up to 50% (Less words, More report!
🎯 Focus: Keep your eyes on the images, not the keyboard!
💸 Revenue: Boost revenue by at least 20%
📑 Clarity: Patient summary in plain English
_Cover_Photo.png)
_Cover_Photo.png)

