Slug
depression
Video
Category
Mood Disorders
Excerpt
Depression, also called major depressive disorder, is a common medical condition that negatively affects how you feel, the way you think, and how you act. Depression causes persistent feelings of sadness and/or a loss of interest in activities you once enjoyed. It can impair your ability to perform at work and at home and cause a number of emotional and physical problems.
Authors
Tags
Featured
Featured
Ready to Publish
Ready to Publish
Publish Date
Dec 7, 2022

What Is Depression?
Depression, also called major depressive disorder, is a common medical condition that negatively affects how you feel, the way you think, and how you act. Depression causes persistent feelings of sadness and/or a loss of interest in activities you once enjoyed. It can impair your ability to perform at work and at home and cause a number of emotional and physical problems.

Symptoms of Depression
Depression symptoms can vary from mild to severe and can include:
- Feeling sadness, tearfulness, or hopelessness
- Angry outbursts, irritability, or frustration, even over small matters
- Loss of interest or pleasure in normal activities, such as sex, hobbies, or sports
- Changes in appetite — weight loss or gain, reduced appetite, or increased craving for food
- Sleep disturbances, including trouble sleeping or sleeping too much
- Lack of energy or increased fatigue, even simple tasks need more effort
- Increase in purposeless physical activity (e.g., inability to sit still, pacing, handwringing) or slowed movements or speech (these actions must be severe enough to be observable by others)
- Feeling worthlessness or guilt, fixating on past failures or self-blame
- Difficulty thinking, concentrating or making decisions
- Thoughts of death or suicide
- Unexplained physical problems, such as back pain or headaches
Depression Symptoms in Children and Teenagers
The typical signs and symptoms of depression in children and teenagers are comparable to those in adults, although there may be some distinctions.
- In younger children, depression may manifest as sadness, irritability, clinginess, worry, aches, and pains, refusal to go to school, or being underweight.
- In teens, symptoms may include sadness, irritability, feeling negative and worthless, anger, poor performance or poor attendance at school, feeling misunderstood and extremely sensitive, using recreational drugs or alcohol, eating or sleeping too much, self-harm, loss of interest in normal activities, and avoidance of social interaction.
Depression Symptoms in Elderly
Depression is not a normal part of growing older, and it should never be taken lightly. Unfortunately, depression often goes undiagnosed and untreated in older adults, and they may be hesitant to seek help. Older persons may experience various or less noticeable signs of depression, such as:
- Memory difficulties or personality changes
- Physical aches or pain
- Fatigue, loss of appetite, sleep problems, or loss of interest in sex — not caused by a medical condition or medication
- Often want to stay at home, rather than go out to socialize or do new things
- Suicidal thinking or feelings, especially in older men
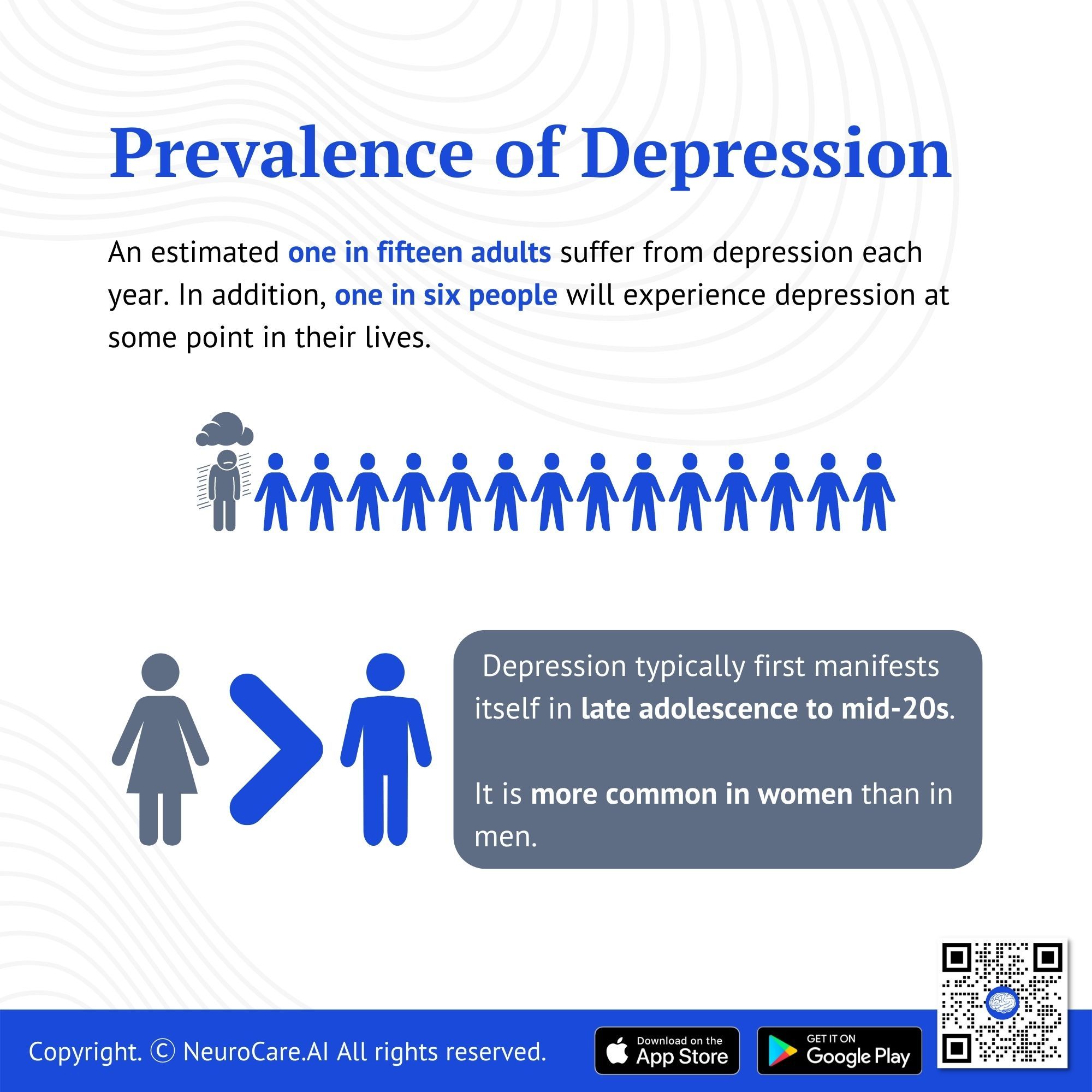
Prevalence of Depression
An estimated one in fifteen adults (6.7%) suffer from depression each year. In addition, one in six people (16.6%) will experience depression at some point in their lives. Although depression can occur at any time, it typically first manifests itself in late adolescence to mid-life. Depression is more common in women than in men. According to some research, one-third of women will go through a major depressive episode at some point in their lives. When first-degree relatives (parents, children, or siblings) also have depression, there is a significant degree of heritability (about 40%).

Depression is More Than Sadness, Grief, or Bereavement
The loss of a loved one, the termination of a job, or the dissolution of a relationship are all trying events for a person to go through. It is common for people to experience sadness or grief in response to such circumstances. People who have lost something frequently label themselves as "depressed.”
But being sad is not the same as being depressed. The grieving process is normal, unique to each person, and shares some characteristics with depression. Depression and grief both have the potential to cause extreme sadness and withdrawal from daily activities, but they differ in several key ways:
- When someone is grieving/bereaving, unpleasant emotions frequently come in waves and are blended with pleasant recollections of the deceased. For the majority of two weeks, mood and/or interest (pleasure) are diminished in serious depression.
- Self-esteem is typically preserved during grieving. Feelings of worthlessness and self-hatred are frequent in major depression.
- In grief/bereavement, thoughts of death may surface when thinking of or fantasizing about “joining” the deceased loved one. In major depression, due to feelings of worthlessness, undeserving of living, or inability to handle the pain of melancholy, thoughts of suicide are common in major depression.
Depression and grief/bereavement can co-exist for some people after losing a loved one, losing their job, becoming the victim of physical violence, or experiencing a significant tragedy. When depression co-exists with grief, the grief is more severe and lasts longer than grief without depression.
Distinguishing between grief/bereavement and depression is important and can help people get the support, care, and treatment they need.

Risk Factors for Depression
What specifically causes depression is unknown. Depression can affect anyone - even those who seem to lead relatively ideal lives. The following factors may contribute to depression:
- Biological differences. People with depression appear to have physical changes in their brains. Although the significance of these changes is still uncertain, they may eventually point to the root causes.
- Brain chemistry. Recent studies suggest that alterations in the neurotransmitters' effects and interactions with the neurocircuits responsible for preserving mood stability may have a substantial impact on depression and its treatment.
- Genetics. Depression can run in families. For instance, if one identical twin develops depression, there is a 70% probability that the other would also get the condition at some point in life.
- Hormones. Depression may be brought on by or triggered by changes in the body’s balance of hormones. Hormone changes can occur during pregnancy, in the days or weeks following delivery (postpartum), and as a result of thyroid issues, menopause, or a variety of other diseases.
- Personality. Depression appears to be more common among people who have low self-esteem, are easily stressed out, or are typically pessimistic.
- Environmental factors. Some people may be more susceptible to depression if they are consistently exposed to violence, neglect, abuse, or poverty.
Complications
Depression is a serious disorder that can have a terrible impact on you and your family. If depression isn't treated, it frequently grows worse, leading to emotional, behavioral, and physiological issues that affect every aspect of your life.
Examples of depression-related problems include:
- Excess weight or obesity, which can lead to heart disease and diabetes
- Pain or physical illness
- Alcohol or drug misuse
- Anxiety, panic disorder, or social phobia
- Family conflicts, relationship difficulties, and work or school problems
- Social isolation
- Suicidal feelings, suicide attempts, or suicide
- Self-mutilation, such as cutting
- Premature death from medical conditions
Prevention
Depression cannot be stopped completely. However, these strategies may help.
- Take action to manage your stress, build your resilience, and improve your self-esteem.
- Reach out to family and friends, especially during times of crisis to get through difficult times.
- Get treatment at the earliest sign of a problem to stop depression from getting worse.
- Think about receiving long-term maintenance treatment to help prevent a relapse of symptoms.

Diagnosis
For a diagnosis of depression, symptoms must persist for at least two weeks and must indicate a change from your pre-existing level of functioning. Additionally, medical conditions like thyroid problems, brain tumors, and vitamin deficiencies can mimic symptoms of depression, so it's important to test out any general medical causes.
Your doctor may determine a diagnosis of depression based on:
- Physical exam. Your doctor may do a physical examination and ask questions about your health. Sometimes a physical health issue may be the underlying cause of depression.
- Lab tests. For instance, your doctor may do a blood test called a complete blood count or check your thyroid to see if it is functioning properly.
- Psychiatric evaluation. Your mental health expert will enquire about your signs, patterns of thought and behavior, and feelings. To assist in addressing these inquiries, you might be requested to complete a questionnaire.
- DSM-5. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) issued by the American Psychiatric Association may be used by your mental health provider to determine whether you meet the criteria for depression.

Treatment for Depression
Depression is among the most treatable mental disorders. Eventually, between 80% and 90% of depressed individuals respond well to therapy. Almost all patients have some symptom alleviation.
Psychotherapy
Psychotherapy, or “talk therapy,” is sometimes used alone for the treatment of mild depression; when treating moderate to severe depression, psychotherapy is frequently combined with antidepressant drugs. Cognitive behavioral therapy (CBT) is a type of psychotherapy that concentrates on fixing problems in the present and it has been found that CBT is successful in treating depression. CBT assists a person in identifying distorted or negative thinking with the aim of altering beliefs and actions to react to difficulties more positively.
Psychotherapy may simply involve the patient, but it may also involve others. Therapy for families or couples, for instance, can assist in addressing problems within these tight bonds. In a safe environment, group therapy brings people with related disorders together, and it can help the participant understand how others handle similar circumstances
The length of treatment depends on how severe the depression is. It may take a few weeks or much more. In many instances, 10 to 15 sessions are sufficient to achieve noticeable progress.
Medication
Brain chemistry may contribute to an individual’s depression and may influence how they are treated. Antidepressants may therefore be prescribed to help alter one's brain chemistry. These drugs are not tranquilizers, sedatives, or "uppers." They do not become habits. Antidepressant drugs typically don't have any stimulating effects on persons who aren't depressed.
The full effects of antidepressants may not become apparent for two to three months after starting treatment. However, they may begin to show some improvement after a week or two. After several weeks, if a patient has made little to no progress, the patient's psychiatrist may adjust the medication's dosage or add or remove another antidepressant. Other psychotropic medicines might be beneficial in some circumstances. If a drug does not function as expected or if you suffer any side effects, you should inform your doctor right once.
After symptoms have improved, psychiatrists typically advise patients to take their medicine for another six months or more. For some individuals at high risk, longer-term maintenance therapy may be advised to reduce the risk of subsequent episodes.
Electroconvulsive Therapy (ECT)
Patients with severe major depression who have not responded to conventional therapies have traditionally been the target population for the medical procedure known as ECT. It involves a brief electrical stimulation of the brain while the patient is under anesthesia. ECT is normally administered to a patient twice to three times per week for a total of six to 12 sessions. The treatment is managed by a team of skilled medical experts, including a psychiatrist, an anesthesiologist, and a nurse. Since the 1940s, ECT has been utilized, and decades of research have resulted in significant advancements and the acceptance of its efficacy as a mainstream therapy rather than a "last resort.”
Self-help and Coping
Depression generally isn't a disorder that you can treat on your own. But in addition to medical care, the following self-care measures can be beneficial:
- Adhere to your treatment plan. Never miss a psychotherapy session or appointment. Do not skip taking your meds, even if you are feeling fine. If you stop, your depressive symptoms may return, and you may also experience withdrawal-like symptoms. Recognize that feeling better will not happen overnight.
- Learn about depression. Learning more about your disease might give you confidence and inspire you to follow your treatment plan. To help them understand and support you, encourage your family to learn about depression.
- Pay attention to warning signs. Learn what can set off your depressive symptoms by consulting your physician or therapist. Plan beforehand so you'll know what to do if your symptoms worsen. Contact your doctor or therapist if you notice any changes in symptoms or how you feel. Ask friends or family to keep an eye out for warning signs.
- Avoid alcohol and recreational drugs. Although it may appear that alcohol or drugs decrease depression symptoms, they typically aggravate symptoms over time and make the condition more difficult to manage. If you require assistance with alcohol or drug usage, speak with your doctor or therapist.
- Take care of yourself. Eat a balanced diet, exercise regularly, and get plenty of sleep. Think about going for a stroll, running, swimming, gardening, or engaging in another enjoyable activity. You need quality sleep for both your physical and emotional health. Consult your doctor about possible solutions if you are having difficulties falling asleep.
When to See a Doctor
There is a treatment for depression, which is a serious condition. The vast majority of depressed persons will recover with the right diagnosis and care. Visit your primary care physician or a psychiatrist as soon as possible if you're showing signs of depression. Talk about your worries and ask for a complete assessment. Your mental health needs are being addressed in this way. If you're hesitant to get help, talk to a friend or family member, a doctor, a member of your religious community, or someone else you can trust.
When to get emergency help
Call 911 in the United States or your local emergency number right away if you think you might hurt yourself or make an attempt at suicide.
Additionally, if you are contemplating suicide, think about these alternatives:
- Call your doctor or mental health professional.
- Contact a suicide hotline.
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader, or someone else in your faith community.
Make sure someone stays with a loved one who is contemplating suicide or has already attempted suicide. Dial your local emergency number or 911 right away. Alternatively, if you believe it to be safe to do so, take the patient to the emergency room of the closest hospital.
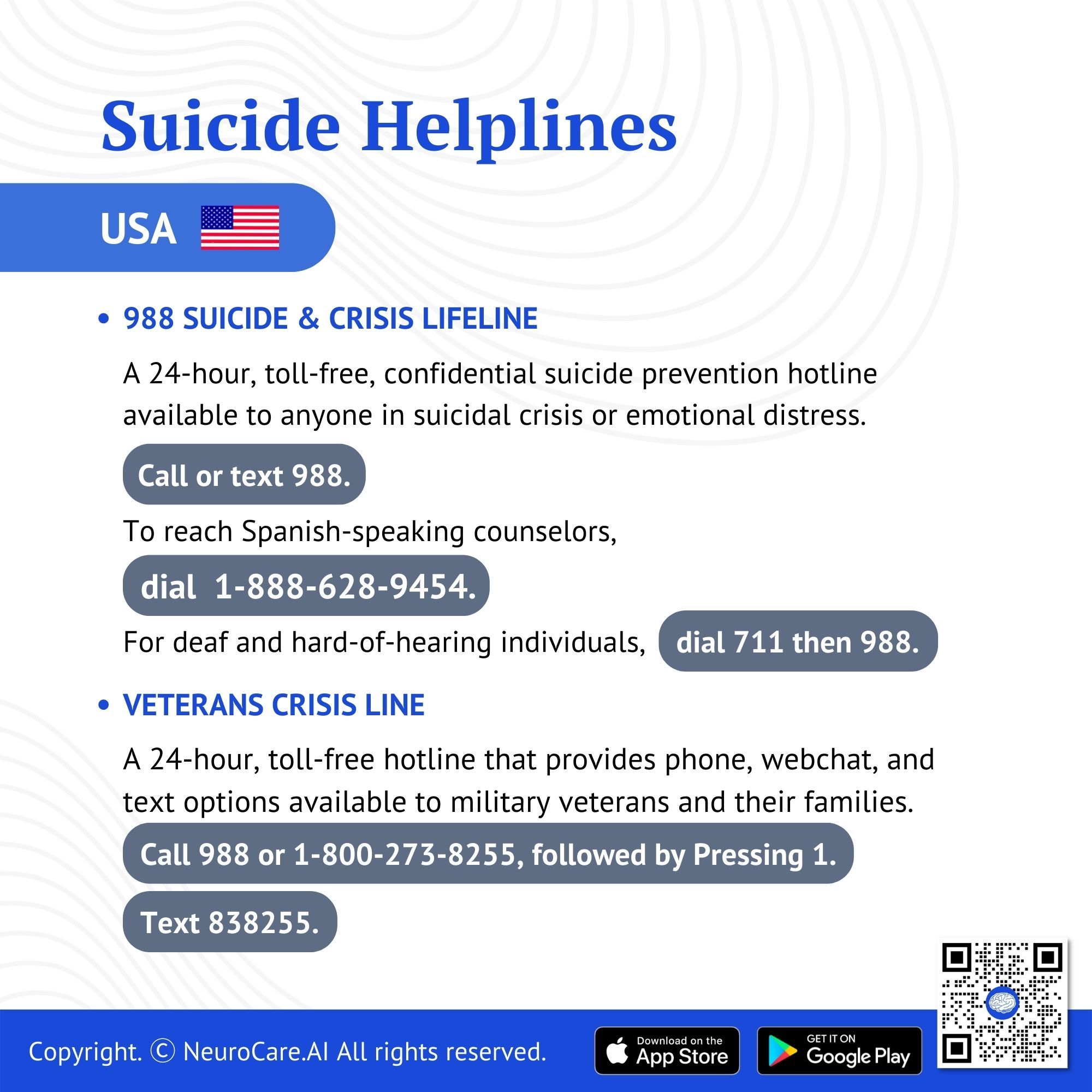
Suicide Helplines
You may reach the following helplines if you have suicidal thoughts and need guidance:
USA
- 988 Suicide & Crisis Lifeline. A 24-hour, toll-free, confidential suicide prevention hotline available to anyone in suicidal crisis or emotional distress.
- Call or text 988.
- To reach Spanish-speaking counselors, dial 1-888-628-9454.
- For deaf and hard-of-hearing individuals, dial 711 and then 988.
- Veterans Crisis Line. A 24-hour, toll-free hotline that provides phone, webchat, and text options available to military veterans and their families.
- Call 988 or 1-800-273-8255, followed by Pressing 1.
- Text 838255.
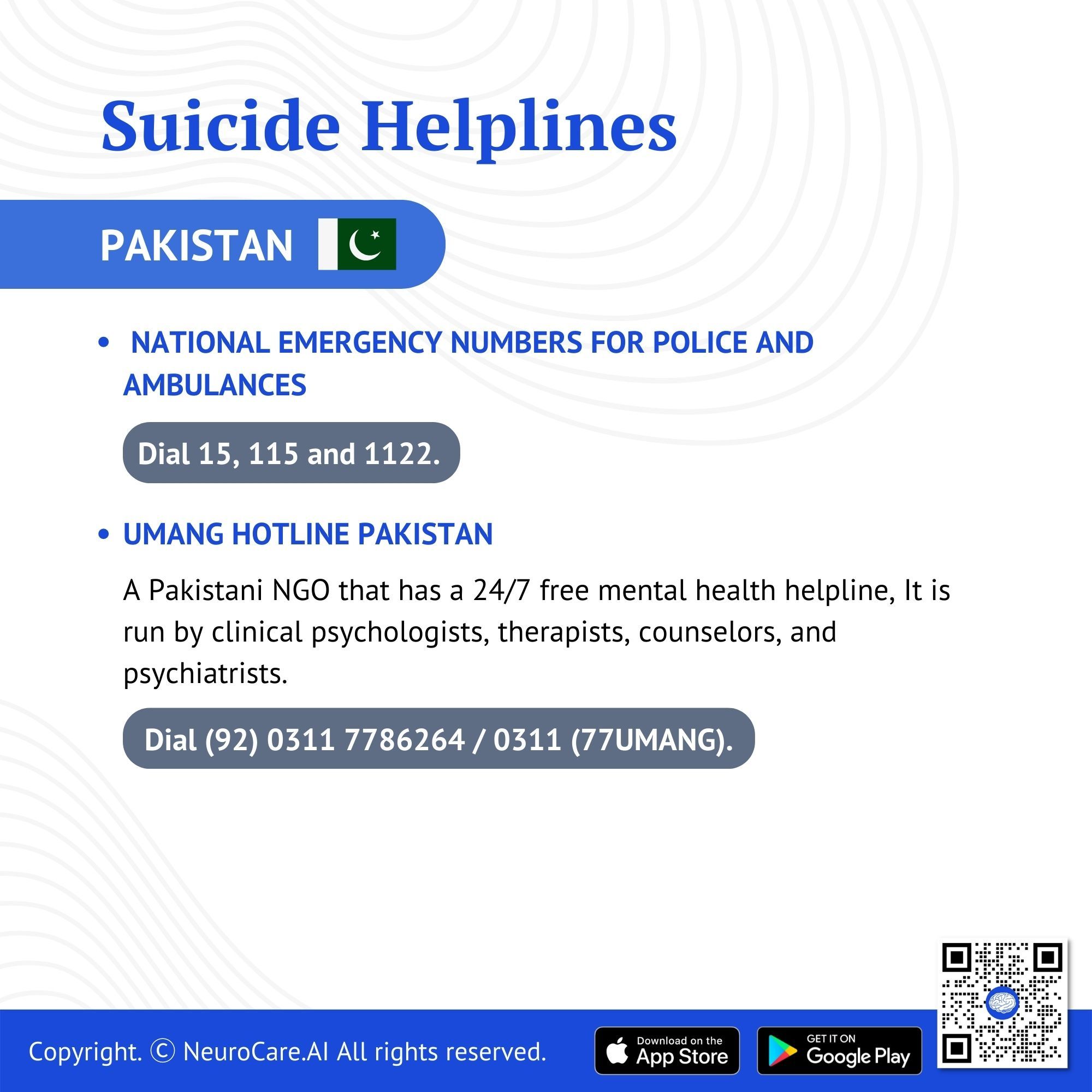
Pakistan
- National Emergency Numbers for Police and Ambulances
- Dial 15, 115 and 1122.
- Umang Hotline Pakistan. A Pakistani NGO that has a 24/7 free mental health helpline, It is run by clinical psychologists, therapists, counselors, and psychiatrists.
- Dial (92) 0311 7786264 / 0311 (77UMANG).
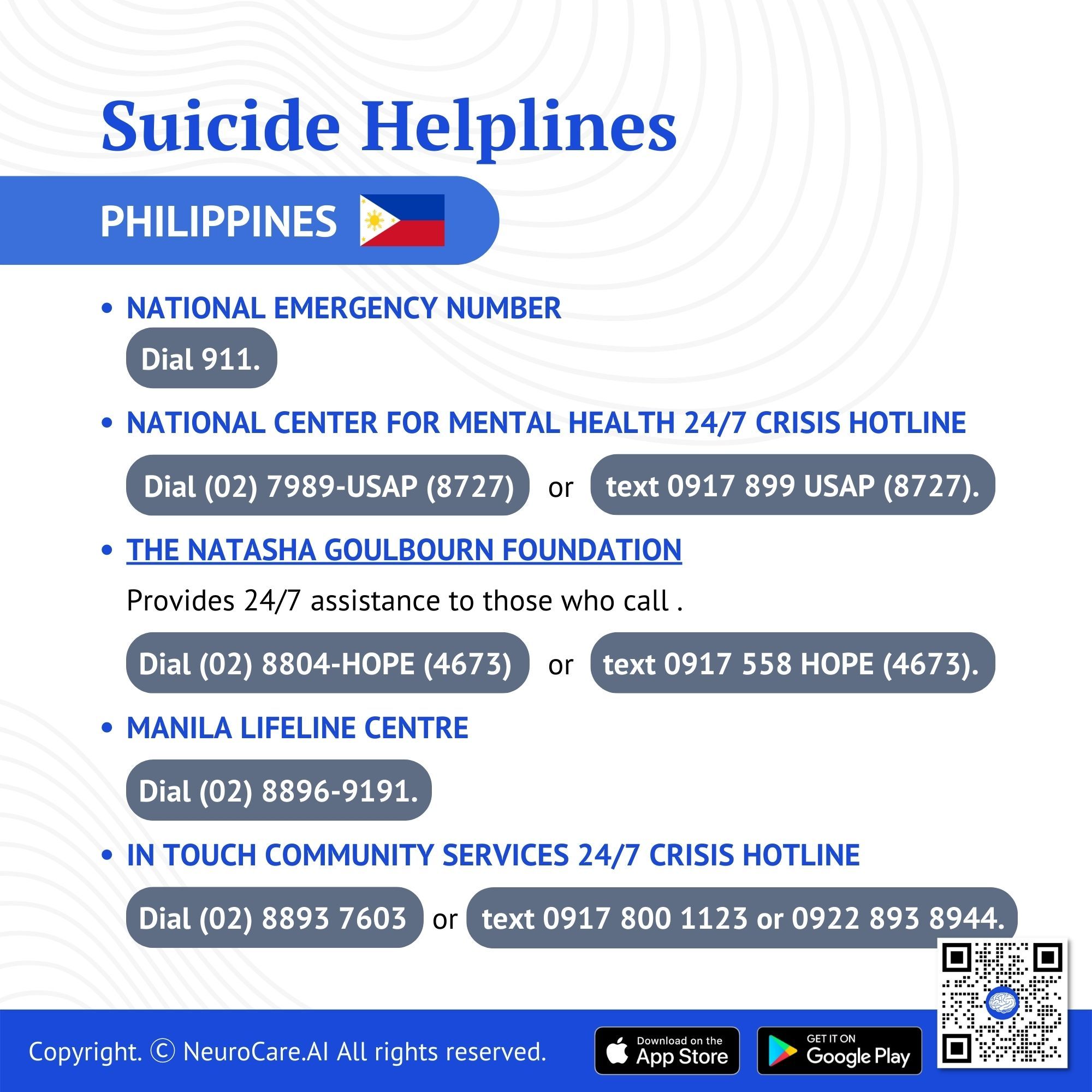
Philippines
- National Emergency Number
- Dial 911.
- National Center for Mental Health 24/7 Crisis Hotline
- Dial (02) 7989-USAP (8727) or 0917 899 USAP (8727).
- The Natasha Goulbourn Foundation. Provides 24/7 assistance to those who call .
- Dial (02) 8804-HOPE (4673)
- Text 0917 558 HOPE (4673).
- Manila Lifeline Centre
- Dial (02) 8896-9191.
- In Touch Community Services 24/7 Crisis Hotline
- Dial (02) 8893 7603
- Text 0917 800 1123 or 0922 893 8944.
Reference:
American Psychiatry Association. (2020). Depression. https://www.psychiatry.org/patients-families/depression/what-is-depression
Mayo Clinic. (n.d.). Depression (Major depressive disorder). https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
World Health Organization. (2021, September 13). Depression. https://www.who.int/news-room/fact-sheets/detail/depression
Wikipedia. (2022, November 20). List of suicide crisis lines. https://en.wikipedia.org/wiki/List_of_suicide_crisis_lines
DISCLAIMER:
The information in this document is for general educational purposes only. It is not intended to substitute for personalized medical professional advice. NeuroCare.AI makes every effort to provide accurate and timely information, but makes no guarantee in this regard and disclaims responsibility for adverse consequences resulting from its use. For further information, consult a physician and the organization referred to herein.
AizaMD™: Revolutionizing Clinical Documentation
Discover the power of our ambient clinical documentation system, designed to transform clinical encounters into structured SOAP notes with unmatched ease. Experience exceptional value for less than $3 per day—cheaper than your daily coffee!
- Save Time: Free up over 90 minutes daily for each provider.
- Boost Revenue: Increase daily revenue by at least $1,000 per provider.
- Enhance Coding Quality: Our detailed documentation supports superior coding accuracy, ensuring optimal reimbursement.
- Maximize Engagement and Interaction: Dedicate more time to patient care and less to typing, fostering richer and more effective conversations between clinicians and patients
AizaMD™: Automated Radiology Report Generation!
Discover our breakthrough Radiology AI reporting platform built on Ambient AI. It enhances productivity and minimizes fatigue. Benefit from best-in-class accuracy with our automated radiology report generation, all at market-leading pricing.
📈 Efficiency: Cut dictation times by up to 50% (Less words, More report!
🎯 Focus: Keep your eyes on the images, not the keyboard!
💸 Revenue: Boost revenue by at least 20%
📑 Clarity: Patient summary in plain English